当前位置:
X-MOL 学术
›
Spinal Cord
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Use of oral third generation cephalosporins and quinolones and occurrence of antibiotic-resistant strains in the neurogenic bladder (NB) outpatient setting: a retrospective chart audit.
Spinal Cord ( IF 2.1 ) Pub Date : 2020-01-21 , DOI: 10.1038/s41393-020-0416-8 Koichi Kitagawa 1, 2 , Katsumi Shigemura 2, 3 , Masashi Nomi 4 , Nozomi Takami 4 , Naoki Yamada 2 , Masato Fujisawa 3
Spinal Cord ( IF 2.1 ) Pub Date : 2020-01-21 , DOI: 10.1038/s41393-020-0416-8 Koichi Kitagawa 1, 2 , Katsumi Shigemura 2, 3 , Masashi Nomi 4 , Nozomi Takami 4 , Naoki Yamada 2 , Masato Fujisawa 3
Affiliation
|
STUDY DESIGN
A retrospective chart audit.
OBJECTIVES
Neurogenic bladder (NB), a risk factor for urinary tract infection, has not been comprehensively studied in terms of antimicrobial stewardship. In this study, we studied the relationship between the use of oral third generation cephalosporins and quinolones, and the occurrence of antibiotic-resistant strains.
SETTING
Hyogo Prefectural Central Rehabilitation Hospital, Hyogo, Japan.
METHODS
We retrospectively investigated antibiotic-resistant bacteria and the amount of antibiotics prescribed in outpatients with NB caused by spinal cord injury between 2012 and 2017. We intervened in urological departments whose physicians often prescribed third generation cephalosporins and fluoroquinolone, and analyzed the number of prescriptions and the amount of Cefdinir (CFDN) and Levofloxacin (LVFX), and studied changes of ratios in antibiotic-resistant strains such as extended-spectrum β-lactamases (ESBLs) and quinolone-resistant Escherichia coli and Klebsiella pneumoniae.
RESULTS
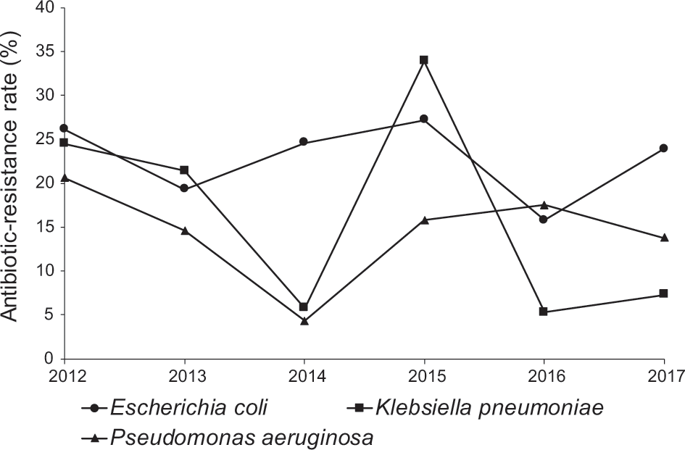
The number of CFDN prescriptions per year significantly decreased from 463 cases to 130 cases over 6 years (p = 0.012). The number of LVFX prescriptions per year decreased from 640 cases to 171 cases (p = 0.025). The incidence rate of ESBL-producing K. pneumoniae decreased from 25% to 7% of total K. pneumoniae (p < 0.001). The incidence of LVFX-resistant E. coli and K. pneumoniae significantly decreased in 2017 compared with 2012 (p = 0.03 and p = 0.016, respectively).
CONCLUSIONS
Antimicrobial stewardship interventions decreased the use of CFDN and LVFX for outpatients with NB. Our findings suggested that the reduction in the use of third generation cephalosporins and quinolones correlates with observed decrease in the occurrence of antibiotic-resistant, ESBL-producing, and quinolone-resistant bacteria.
中文翻译:

口服第三代头孢菌素和喹诺酮类药物的使用以及神经原性膀胱(NB)门诊患者中抗生素耐药菌株的发生:回顾性图表审核。
研究设计回顾性图表审计。目的神经源性膀胱(NB)是泌尿道感染的危险因素,尚未就抗菌素管理进行全面研究。在这项研究中,我们研究了口服第三代头孢菌素和喹诺酮类药物与抗生素耐药菌株的发生之间的关系。地点日本兵库县兵库县中央康复医院。方法我们回顾性调查了2012年至2017年之间因脊髓损伤而导致的NB门诊患者的耐药菌和处方抗生素的使用情况。我们干预了泌尿科,其医生经常开处方第三代头孢菌素和氟喹诺酮,并分析了处方数量和头孢地尼(CFDN)和左氧氟沙星(LVFX)的量,并研究了抗药性菌株(如广谱β-内酰胺酶(ESBLs)和耐喹诺酮类大肠杆菌和肺炎克雷伯菌)的比率变化。结果在6年中,每年CFDN处方数量从463例减少到130例(p = 0.012)。每年LVFX处方的数量从640例减少到171例(p = 0.025)。产生ESBL的肺炎克雷伯菌的发生率从总肺炎克雷伯菌的25%降至7%(p <0.001)。与2012年相比,2017年耐LVFX的大肠埃希菌和肺炎克雷伯菌的发生率显着下降(分别为p = 0.03和p = 0.016)。结论抗菌药物干预减少了NB门诊患者使用CFDN和LVFX。
更新日期:2020-01-21
中文翻译:

口服第三代头孢菌素和喹诺酮类药物的使用以及神经原性膀胱(NB)门诊患者中抗生素耐药菌株的发生:回顾性图表审核。
研究设计回顾性图表审计。目的神经源性膀胱(NB)是泌尿道感染的危险因素,尚未就抗菌素管理进行全面研究。在这项研究中,我们研究了口服第三代头孢菌素和喹诺酮类药物与抗生素耐药菌株的发生之间的关系。地点日本兵库县兵库县中央康复医院。方法我们回顾性调查了2012年至2017年之间因脊髓损伤而导致的NB门诊患者的耐药菌和处方抗生素的使用情况。我们干预了泌尿科,其医生经常开处方第三代头孢菌素和氟喹诺酮,并分析了处方数量和头孢地尼(CFDN)和左氧氟沙星(LVFX)的量,并研究了抗药性菌株(如广谱β-内酰胺酶(ESBLs)和耐喹诺酮类大肠杆菌和肺炎克雷伯菌)的比率变化。结果在6年中,每年CFDN处方数量从463例减少到130例(p = 0.012)。每年LVFX处方的数量从640例减少到171例(p = 0.025)。产生ESBL的肺炎克雷伯菌的发生率从总肺炎克雷伯菌的25%降至7%(p <0.001)。与2012年相比,2017年耐LVFX的大肠埃希菌和肺炎克雷伯菌的发生率显着下降(分别为p = 0.03和p = 0.016)。结论抗菌药物干预减少了NB门诊患者使用CFDN和LVFX。











































 京公网安备 11010802027423号
京公网安备 11010802027423号