当前位置:
X-MOL 学术
›
Spinal Cord
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Scoliosis in paediatric onset spinal cord injuries.
Spinal Cord ( IF 2.1 ) Pub Date : 2020-01-20 , DOI: 10.1038/s41393-020-0418-6 R Kulshrestha 1 , J H Kuiper 1 , W El Masri 2 , J R Chowdhury 1 , S Kaur 1 , N Kumar 1 , R Lalam 1 , A E Osman 1
Spinal Cord ( IF 2.1 ) Pub Date : 2020-01-20 , DOI: 10.1038/s41393-020-0418-6 R Kulshrestha 1 , J H Kuiper 1 , W El Masri 2 , J R Chowdhury 1 , S Kaur 1 , N Kumar 1 , R Lalam 1 , A E Osman 1
Affiliation
|
STUDY DESIGN
This is a retrospective longitudinal review.
OBJECTIVE
The purpose of this review was to identify predictors of developing clinical scoliosis and compare between traumatic and neurological aetiologies of SCI.
SETTING
This study was conducted at the Midland Centre of SCI.
METHOD
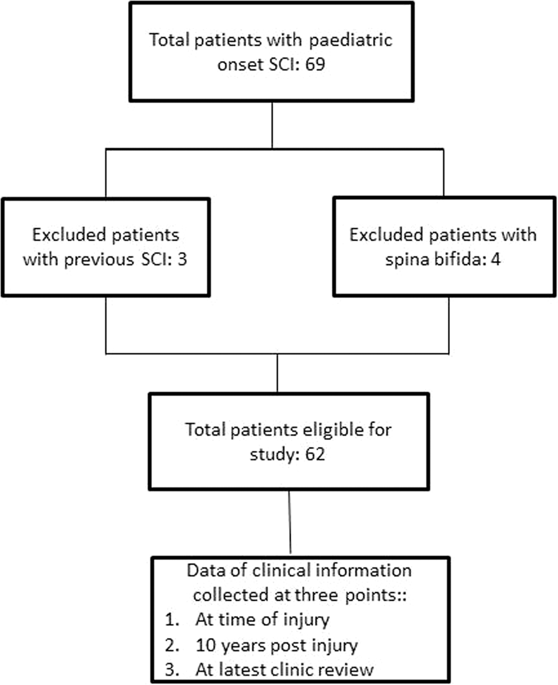
Case notes of all patients injured at an age up to 18 years and admitted between 1971 and 2013 were reviewed.
RESULTS
Sixty-nine individuals were identified, of which seven were excluded: three with pre-existing scoliosis and four with spina bifida. The remaining 62 (44 males, 18 females) had a median age at injury of 17 years (inter quartile range 13-17). Of these, 51 (82%) had traumatic and 11 (18%) had neurological injury. Most (42/51; 82%) of the children who had a traumatic injury were older than 13 years. The risk of developing scoliosis was lower for older patients (RR 0.68 per year, 95% CI 0.52-0.83) or following a traumatic injury (RR 0.36, 95% CI 0.20-0.66). A multivariable analysis based on age and trauma showed that only older age decreased the risk. A robust Receiver Operator Curve analysis suggested 14.6 years as the optimal threshold to predict development of scoliosis within 10 years (Area Under the Curve; AUC 0.83 (95% CI 0.73-0.93), sensitivity 70% (95% CI 50-89%), specificity 89% (95% CI 74-100%).
CONCLUSION
Our results suggest that age below 14.6 years was a predictor for scoliosis. Once adjustment is made for age, the incidence of scoliosis does not differ between traumatic and neurological aetiologies of paediatric SCI injury.
中文翻译:

小儿脊柱侧弯起病于脊髓损伤。
研究设计这是一项回顾性纵向审查。目的本综述的目的是确定临床脊柱侧凸发展的预测因素,并比较SCI的创伤性和神经性病因。设置本研究在SCI的Midland中心进行。方法回顾性分析了1971年至2013年之间18岁以下且入院的所有患者的病例记录。结果确定了69例个体,其中排除了7例:3例既有脊柱侧弯和4例脊柱裂。其余62位(男性44位,女性18位)受伤时的平均年龄为17岁(四分位间距13-17)。其中,有51名(82%)受了创伤,有11名(18%)受了神经病。大多数(42/51; 82%)遭受外伤的儿童年龄大于13岁。老年患者(每年RR 0.68,95%CI 0.52-0.83)或外伤后发生脊柱侧弯的风险较低(RR 0.36,95%CI 0.20-0.66)。基于年龄和创伤的多变量分析表明,只有年龄较大的人才能降低风险。强大的接收器操作员曲线分析建议以14.6年作为预测10年内脊柱侧弯发展的最佳阈值(曲线下面积; AUC 0.83(95%CI 0.73-0.93),灵敏度70%(95%CI 50-89%) ,特异性89%(95%CI 74-100%)结论我们的结果表明年龄在14.6岁以下是脊柱侧弯的预测因素,对年龄进行调整后,儿童的创伤性和神经性病因在脊柱侧弯的发生率上没有差异。 SCI伤害。20-0.66)。基于年龄和创伤的多变量分析表明,只有年龄较大的人才能降低风险。强大的接收器操作员曲线分析建议以14.6年作为预测10年内脊柱侧弯发展的最佳阈值(曲线下面积; AUC 0.83(95%CI 0.73-0.93),灵敏度70%(95%CI 50-89%) ,特异性89%(95%CI 74-100%)结论我们的结果表明年龄在14.6岁以下是脊柱侧弯的预测因素,对年龄进行调整后,儿童的创伤性和神经性病因在脊柱侧弯的发生率上没有差异。 SCI伤害。20-0.66)。基于年龄和创伤的多变量分析表明,只有年龄较大的人才能降低风险。强大的接收器操作员曲线分析建议14.6年作为预测10年内脊柱侧弯发展的最佳阈值(曲线下面积; AUC 0.83(95%CI 0.73-0.93),灵敏度70%(95%CI 50-89%) ,特异性89%(95%CI 74-100%)结论我们的结果表明年龄在14.6岁以下是脊柱侧弯的预测因素,对年龄进行调整后,儿童的创伤性和神经性病因在脊柱侧弯的发生率上没有差异SCI损伤。
更新日期:2020-01-20
中文翻译:

小儿脊柱侧弯起病于脊髓损伤。
研究设计这是一项回顾性纵向审查。目的本综述的目的是确定临床脊柱侧凸发展的预测因素,并比较SCI的创伤性和神经性病因。设置本研究在SCI的Midland中心进行。方法回顾性分析了1971年至2013年之间18岁以下且入院的所有患者的病例记录。结果确定了69例个体,其中排除了7例:3例既有脊柱侧弯和4例脊柱裂。其余62位(男性44位,女性18位)受伤时的平均年龄为17岁(四分位间距13-17)。其中,有51名(82%)受了创伤,有11名(18%)受了神经病。大多数(42/51; 82%)遭受外伤的儿童年龄大于13岁。老年患者(每年RR 0.68,95%CI 0.52-0.83)或外伤后发生脊柱侧弯的风险较低(RR 0.36,95%CI 0.20-0.66)。基于年龄和创伤的多变量分析表明,只有年龄较大的人才能降低风险。强大的接收器操作员曲线分析建议以14.6年作为预测10年内脊柱侧弯发展的最佳阈值(曲线下面积; AUC 0.83(95%CI 0.73-0.93),灵敏度70%(95%CI 50-89%) ,特异性89%(95%CI 74-100%)结论我们的结果表明年龄在14.6岁以下是脊柱侧弯的预测因素,对年龄进行调整后,儿童的创伤性和神经性病因在脊柱侧弯的发生率上没有差异。 SCI伤害。20-0.66)。基于年龄和创伤的多变量分析表明,只有年龄较大的人才能降低风险。强大的接收器操作员曲线分析建议以14.6年作为预测10年内脊柱侧弯发展的最佳阈值(曲线下面积; AUC 0.83(95%CI 0.73-0.93),灵敏度70%(95%CI 50-89%) ,特异性89%(95%CI 74-100%)结论我们的结果表明年龄在14.6岁以下是脊柱侧弯的预测因素,对年龄进行调整后,儿童的创伤性和神经性病因在脊柱侧弯的发生率上没有差异。 SCI伤害。20-0.66)。基于年龄和创伤的多变量分析表明,只有年龄较大的人才能降低风险。强大的接收器操作员曲线分析建议14.6年作为预测10年内脊柱侧弯发展的最佳阈值(曲线下面积; AUC 0.83(95%CI 0.73-0.93),灵敏度70%(95%CI 50-89%) ,特异性89%(95%CI 74-100%)结论我们的结果表明年龄在14.6岁以下是脊柱侧弯的预测因素,对年龄进行调整后,儿童的创伤性和神经性病因在脊柱侧弯的发生率上没有差异SCI损伤。











































 京公网安备 11010802027423号
京公网安备 11010802027423号