The Lancet Global Health ( IF 19.9 ) Pub Date : 2020-01-17 , DOI: 10.1016/s2214-109x(19)30546-7 Nguyen Toan Tran 1 , Armando Seuc 2 , Béatrice Tshikaya 3 , Maurice Mutuale 4 , Sihem Landoulsi 2 , Brigitte Kini 5 , Bernadette Mbu Nkolomonyi 5 , Jean Nyandwe Kyloka 4 , Félicité Langwana 4 , Asa Cuzin-Kihl 2 , James Kiarie 2 , Mary Eluned Gaffield 2 , Rachel Yodi 3 , Désiré Mashinda Kulimba 4
|
Background
In rural Burkina Faso, a package of six low-technology, post-partum contraceptive interventions (ie, refresher training for providers, a counselling tool, supportive supervision, daily availability of contraceptive services, client appointment cards, and invitation letters to attend appointments for partners), aimed at strengthening existing primary health-care services and enhancing demand for them, doubled the use of modern contraceptives at 12 months post partum (ie, 55% uptake in intervention recipients vs 29% in routine-care users). This study assessed the effect of a similar package but in urban settings of Kinshasa province, Democratic Republic of the Congo, in an effort to reduce the unmet need for post-partum family planning.
Methods
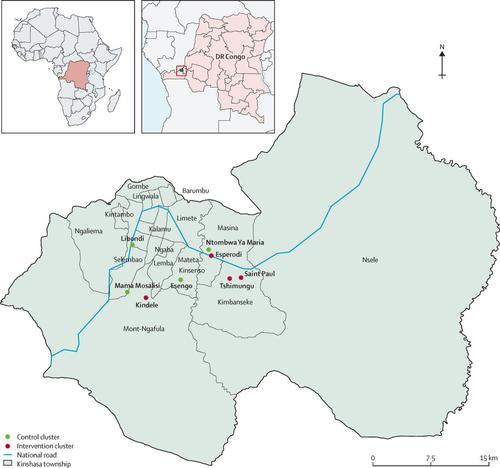
Yam Daabo was a multi-intervention, single-blinded, cluster-randomised controlled trial done in six primary health-care centres (clusters) in Kinshasa. Centres were randomly allocated to receive the six-component intervention or standard antenatal and postnatal care in matched pairs (1:1) on the basis of number of monthly births, the ratio of health workers per population in the health zone, and the urban and suburban settings. Only data analysts could be masked to cluster allocation. Health-care facilities were eligible if they provided a continuum of antenatal, delivery, and postnatal care, were well stocked with contraceptives, and were situated close to the main study centre. All pregnant women presenting to the six centres were eligible if they were in their third pregnancy trimester and had no counterindications to deliver in the facility. The main outcome was prevalence of use of modern contraceptives at 12 months after delivery. Analysis was by modified intention-to-treat using generalised linear mixed models or Fisher's exact test for small groups. Prevalence ratios were adjusted for cluster effects and baseline characteristics. This study was registered with the Pan-African Clinical Trials Registry (PACTR201609001784334).
Findings
From July 1, 2016, to Feb 2, 2017, eight of 52 clinics assessed for eligibility met the criteria and were randomised. Of 690 women approached, 576 (83%) women were enrolled: 286 in the four intervention clusters and 290 in the four control clusters. Of them, 519 (90%) completed the 12-month study exit interview (252 in the intervention group and 267 in the control group) and were included in the intention-to-treat analysis. At 12 months, 115 (46%) of 252 women in the intervention group and 94 (35%) of 267 in the control group were using modern contraceptives (adjusted prevalence ratio [PR] 1·58, 95% CI 0·74–3·38), with significant differences in the use of contraceptive implants (22% vs 6%; adjusted PR 4·36, 95% CI 1·96–9·70), but without difference in the use of short-acting contraceptives (23% vs 28%; 0·92, 0·29–2·98) and non-modern or inappropriate methods (7% vs 18%; 0·45, 0·13–1·54). There were no serious adverse events or maternal deaths related to the study.
Interpretation
The Yam Daabo intervention package did not have a significant effect on the overall use of effective modern contraceptives but significantly increased implant use in women post partum who live in urban settings in Kinshasa up to a year after childbirth. However, interferences from external family planning initiatives in the control group might have diminished differences between the services received. Such an intervention could be potentially relevant in similar contexts in DR Congo and other countries.
Funding
Government of France; UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction.
中文翻译:

刚果民主共和国金沙萨 (Yam Daabo) 产后计划生育干预对分娩后 1 年避孕药具使用和方法组合的有效性:一项单盲、整群随机对照试验。
背景
在布基纳法索农村地区,一揽子六种低技术产后避孕干预措施(即对服务提供者的进修培训、咨询工具、支持性监督、每日提供的避孕服务、客户预约卡和参加预约的邀请函)合作伙伴)旨在加强现有的初级卫生保健服务并增加对这些服务的需求,将产后 12 个月时现代避孕药具的使用率增加了一倍(即干预接受者的使用率为 55% ,而常规护理使用者的使用率为 29%)。这项研究评估了刚果民主共和国金沙萨省城市环境中类似一揽子计划的效果,以减少未满足的产后计划生育需求。
方法
Yam Daabo 是一项多干预、单盲、整群随机对照试验,在金沙萨的六个初级卫生保健中心(集群)进行。根据每月出生人数、卫生区卫生人员与人口的比例、城市和城市的情况,按配对(1:1)随机分配中心接受六项干预或标准产前和产后护理。郊区设置。只有数据分析师才能隐藏集群分配的情况。如果卫生保健机构提供连续的产前、分娩和产后护理,备有充足的避孕药具,并且位于主要研究中心附近,则符合资格。所有到这六个中心就诊的孕妇如果处于妊娠晚期并且没有在该机构分娩的禁忌症,则符合资格。主要结果是产后 12 个月时现代避孕药具的使用率。分析是通过使用广义线性混合模型或针对小组的费舍尔精确检验进行修改的意向治疗进行的。根据集群效应和基线特征调整患病率。该研究已在泛非临床试验注册中心注册(PACTR201609001784334)。
发现
从2016年7月1日到2017年2月2日,接受资格评估的52家诊所中有8家符合标准并被随机分组。在 690 名接受咨询的女性中,有 576 名 (83%) 女性被登记:4 个干预组中 286 名女性,4 个对照组中 290 名女性。其中,519 人(90%)完成了为期 12 个月的研究退出访谈(干预组 252 人,对照组 267 人)并被纳入意向治疗分析。 12 个月时,干预组 252 名女性中的 115 名 (46%) 和对照组 267 名女性中的 94 名 (35%) 使用现代避孕药具(调整后的患病率 [PR] 1·58,95% CI 0·74– 3·38),皮下埋植避孕药的使用存在显着差异(22% vs 6%;调整后 PR 4·36,95% CI 1·96–9·70),但短效避孕药的使用没有差异(23% vs 28%;0·92、0·29–2·98)和非现代或不适当的方法(7% vs 18%;0·45、0·13–1·54)。没有与该研究相关的严重不良事件或孕产妇死亡。
解释
Yam Daabo 干预方案对有效现代避孕药具的总体使用没有显着影响,但显着增加了居住在金沙萨城市环境中的妇女产后一年内埋植剂的使用。然而,对照组中外部计划生育举措的干扰可能会缩小所接受服务之间的差异。这种干预措施可能对刚果民主共和国和其他国家的类似情况具有潜在意义。
资金
法国政府;联合国开发计划署/联合国人口基金/联合国儿童基金会/世界卫生组织/世界银行人类生殖研究、发展和研究培训特别规划。











































 京公网安备 11010802027423号
京公网安备 11010802027423号