当前位置:
X-MOL 学术
›
JAMA Psychiatry
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Risk of Subjection to Violence and Perpetration of Violence in Persons With Psychiatric Disorders in Sweden.
JAMA Psychiatry ( IF 22.5 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamapsychiatry.2019.4275 Amir Sariaslan 1, 2 , Louise Arseneault 3 , Henrik Larsson 4, 5 , Paul Lichtenstein 4 , Seena Fazel 1
JAMA Psychiatry ( IF 22.5 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamapsychiatry.2019.4275 Amir Sariaslan 1, 2 , Louise Arseneault 3 , Henrik Larsson 4, 5 , Paul Lichtenstein 4 , Seena Fazel 1
Affiliation
|
Importance
Key outcomes for persons with psychiatric disorders include subjection to violence and perpetration of violence. The occurrence of these outcomes and their associations with psychiatric disorders need to be clarified.
Objective
To estimate the associations of a wide range of psychiatric disorders with the risks of subjection to violence and perpetration of violence.
Design, Setting, and Participants
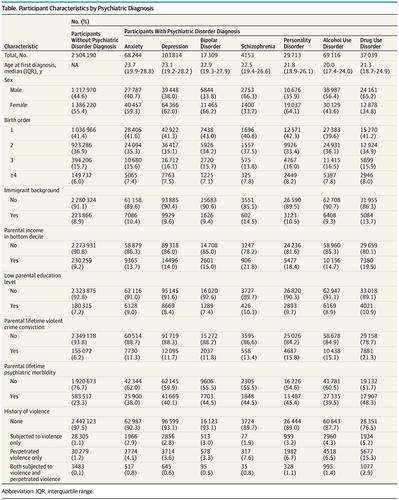
A total of 250 419 individuals born between January 1, 1973, and December 31, 1993, were identified to have psychiatric disorders using Swedish nationwide registers. Premorbid subjection to violence was measured since birth. The patients were matched by age and sex to individuals in the general population (n = 2 504 190) and to their full biological siblings without psychiatric disorders (n = 194 788). The start date for the patients and control groups was defined as the discharge date of the first psychiatric episode. The participants were censored either when they migrated, died, experienced the outcome of interest, or reached the end of the study period on December 31, 2013. Data were analyzed from January 15 to September 14, 2019.
Exposures
Patients with common psychiatric disorders (eg, schizophrenia, bipolar disorder, depression, and anxiety) were differentiated using a hierarchical approach. Patients with personality disorders and substance use disorders were also included.
Main Outcomes and Measures
Subjection to violence was defined as an outpatient visit (excluding a primary care visit), inpatient episode, or death associated with any diagnosis of an injury that was purposefully inflicted by other persons. Perpetration of violence was defined as a violent crime conviction. Stratified Cox regression models were fitted to account for the time at risk, a range of sociodemographic factors, a history of violence, and unmeasured familial confounders (via sibling comparisons).
Results
Among 250 419 patients (55.4% women), the median (interquartile range) age at first diagnosis ranged from 20.0 (17.4-24.0) years for alcohol use disorder to 23.7 (19.9-28.8) years for anxiety disorder. Compared with 2 504 190 matched individuals without psychiatric disorders from the general population, patients with psychiatric disorders were more likely to be subjected to violence (7.1 [95% CI, 6.9-7.2] vs 7.5 [95% CI, 7.4-7.6] per 1000 person-years) and to perpetrate violence (1.0 [95% CI, 0.9-1.0] vs 0.7 [95% CI, 0.7-0.7] per 1000 person-years). In the fully adjusted models, patients with psychiatric disorders were 3 to 4 times more likely than their siblings without psychiatric disorders to be either subjected to violence (adjusted hazard ratio [aHR], 3.4 [95% CI, 3.2-3.6]) or to perpetrate violence (aHR, 4.2 [95% CI, 3.9-4.4]). Diagnosis with any of the specific disorders was associated with higher rates of violent outcomes, with the sole exception of schizophrenia, which was not associated with the risk of subjection to violence.
Conclusions and Relevance
In this study, persons with psychiatric disorders were 3 to 4 times more likely than their siblings without psychiatric disorders to have been subjected to violence or to have perpetrated violence after the onset of their conditions. The risks of both outcomes varied by specific psychiatric diagnosis, history of violence, and familial risks. Clinical interventions may benefit from targeted approaches for the assessment and management of risk of violence in people with psychiatric disorders.
中文翻译:

瑞典患有精神疾病的人遭受暴力和暴力侵害的风险。
重要性精神病患者的主要结局包括遭受暴力和实施暴力。这些结果的发生及其与精神疾病的关系需要弄清楚。目的评估广泛的精神疾病与遭受暴力和暴力行为风险的关联。设计,环境和参与者根据瑞典全国性登记表,总共1973年1月1日至1993年12月31日之间出生的250 419个人被确定患有精神疾病。自出生以来就测量了病态前的暴力行为。按年龄和性别将患者与普通人群中的个体(n = 2 504 190)和没有精神病的全生物学同胞相匹配(n = 194 788)。患者和对照组的开始日期定义为第一次精神病发作的出院日期。参与者在迁移,死亡,经历感兴趣的结果或达到研究期末时于2013年12月31日进行了审查。对数据的分析时间为2019年1月15日至9月14日。暴露患有常见精神病的患者(例如,精神分裂症,双相情感障碍,抑郁和焦虑)使用分级方法进行区分。人格障碍和药物滥用障碍的患者也包括在内。主要结果和措施遭受暴力的定义是:门诊就诊(不包括基层医疗就诊),住院发作或与诊断为他人故意造成的伤害相关的死亡。暴力行为被定义为暴力犯罪定罪。分层的Cox回归模型适用于考虑风险时间,一系列社会人口统计学因素,暴力史以及无法衡量的家族混杂因素(通过同级比较)。结果在250 419名患者(55.4%的女性)中,初次诊断的中位年龄(四分位间距)为酒精使用障碍的20.0(17.4-24.0)岁至焦虑症的23.7(19.9-28.8)岁。与普通人群中没有精神障碍的2 504 190个匹配个体相比,精神障碍患者更容易遭受暴力侵害(每[7.1 [95%CI,6.9-7.2] vs 7.5 [95%CI,7.4-7.6] 1000人年)和实施暴力行为(每1000人年1.0 [95%CI,0.9-0.7] [0.7 [95%CI,0.7-0.7])。在完全调整的模型中,患有精神疾病的患者遭受暴力的可能性比没有精神疾病的兄弟姐妹高3至4倍(调整后的危险比[aHR],3.4 [95%CI,3.2-3.6])或暴力(aHR,4.2 [95%CI,3.9-4.4])。除精神分裂症外,任何特定疾病的诊断均与较高的暴力结果发生率有关,而精神分裂症则与暴力风险无关。结论与相关性在这项研究中,患有精神疾病的人遭受暴力侵害或在患病后遭受暴力的可能性比没有精神疾病的兄弟姐妹高3至4倍。两种结果的风险因具体的精神病学诊断,暴力史,和家庭风险。临床干预措施可能受益于针对精神疾病患者的暴力风险评估和管理的针对性方法。
更新日期:2020-04-01
中文翻译:

瑞典患有精神疾病的人遭受暴力和暴力侵害的风险。
重要性精神病患者的主要结局包括遭受暴力和实施暴力。这些结果的发生及其与精神疾病的关系需要弄清楚。目的评估广泛的精神疾病与遭受暴力和暴力行为风险的关联。设计,环境和参与者根据瑞典全国性登记表,总共1973年1月1日至1993年12月31日之间出生的250 419个人被确定患有精神疾病。自出生以来就测量了病态前的暴力行为。按年龄和性别将患者与普通人群中的个体(n = 2 504 190)和没有精神病的全生物学同胞相匹配(n = 194 788)。患者和对照组的开始日期定义为第一次精神病发作的出院日期。参与者在迁移,死亡,经历感兴趣的结果或达到研究期末时于2013年12月31日进行了审查。对数据的分析时间为2019年1月15日至9月14日。暴露患有常见精神病的患者(例如,精神分裂症,双相情感障碍,抑郁和焦虑)使用分级方法进行区分。人格障碍和药物滥用障碍的患者也包括在内。主要结果和措施遭受暴力的定义是:门诊就诊(不包括基层医疗就诊),住院发作或与诊断为他人故意造成的伤害相关的死亡。暴力行为被定义为暴力犯罪定罪。分层的Cox回归模型适用于考虑风险时间,一系列社会人口统计学因素,暴力史以及无法衡量的家族混杂因素(通过同级比较)。结果在250 419名患者(55.4%的女性)中,初次诊断的中位年龄(四分位间距)为酒精使用障碍的20.0(17.4-24.0)岁至焦虑症的23.7(19.9-28.8)岁。与普通人群中没有精神障碍的2 504 190个匹配个体相比,精神障碍患者更容易遭受暴力侵害(每[7.1 [95%CI,6.9-7.2] vs 7.5 [95%CI,7.4-7.6] 1000人年)和实施暴力行为(每1000人年1.0 [95%CI,0.9-0.7] [0.7 [95%CI,0.7-0.7])。在完全调整的模型中,患有精神疾病的患者遭受暴力的可能性比没有精神疾病的兄弟姐妹高3至4倍(调整后的危险比[aHR],3.4 [95%CI,3.2-3.6])或暴力(aHR,4.2 [95%CI,3.9-4.4])。除精神分裂症外,任何特定疾病的诊断均与较高的暴力结果发生率有关,而精神分裂症则与暴力风险无关。结论与相关性在这项研究中,患有精神疾病的人遭受暴力侵害或在患病后遭受暴力的可能性比没有精神疾病的兄弟姐妹高3至4倍。两种结果的风险因具体的精神病学诊断,暴力史,和家庭风险。临床干预措施可能受益于针对精神疾病患者的暴力风险评估和管理的针对性方法。











































 京公网安备 11010802027423号
京公网安备 11010802027423号