当前位置:
X-MOL 学术
›
JACC Cardiovasc. Inte.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Transcatheter ViV Versus Redo Surgical AVR for the Management of Failed Biological Prosthesis: Early and Late Outcomes in a Propensity-Matched Cohort.
JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2020-01-09 , DOI: 10.1016/j.jcin.2019.10.030 Derrick Y Tam 1 , Christoffer Dharma 2 , Rodolfo V Rocha 3 , Maral Ouzounian 3 , Harindra C Wijeysundera 4 , Peter C Austin 5 , Joanna Chikwe 6 , Mario Gaudino 7 , Stephen E Fremes 1
JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2020-01-09 , DOI: 10.1016/j.jcin.2019.10.030 Derrick Y Tam 1 , Christoffer Dharma 2 , Rodolfo V Rocha 3 , Maral Ouzounian 3 , Harindra C Wijeysundera 4 , Peter C Austin 5 , Joanna Chikwe 6 , Mario Gaudino 7 , Stephen E Fremes 1
Affiliation
|
OBJECTIVES
The aim of this study was to compare early and late outcomes between redo surgical aortic valve replacement (AVR) and valve-in-valve (ViV) transcatheter AVR.
BACKGROUND
Published studies to date comparing redo surgical AVR (RS) with ViV transcatheter AVR for failed biological prostheses have been small and limited to early outcomes.
METHODS
Clinical and administrative databases for Ontario, Canada's most populous province, were linked to obtain patients undergoing ViV and RS for failed previous biological prostheses. Propensity score matching was performed to account for differences in baseline characteristics. Early outcomes were compared using the McNemar test. Late mortality was compared between the matched groups using a Cox proportional hazards model.
RESULTS
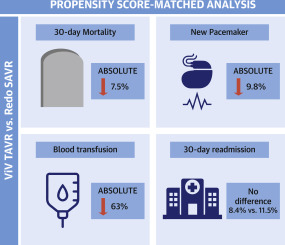
A total of 558 patients undergoing intervention for failed biological prostheses between March 31, 2008, and September 30, 2017, at 11 Ontario institutions (ViV, n = 214; RS, n = 344) were included. Patients who underwent ViV were older and had more comorbidities. Propensity matching on 27 variables yielded similar groups for comparison (n = 131 pairs). Mean time from initial AVR to RS or ViV was 8.6 ± 4.4 years and 11.3 ± 4.5 years, respectively. Thirty-day mortality was significantly lower with ViV compared with RS (absolute risk difference: -7.5%; 95% confidence interval: -12.6% to -2.3%). The rates of permanent pacemaker implantation and blood transfusions were also lower with ViV, as was length of stay. Survival at 5 years was higher with ViV (76.8% vs. 66.8%; hazard ratio: 0.55; 95% confidence interval: 0.30 to 0.99; p = 0.04).
CONCLUSIONS
ViV TAVR was associated with lower early mortality, morbidity, and length of hospital stay and with increased survival compared with RS and may be the preferred approach for the treatment of failed biological prostheses.
中文翻译:

经导管ViV与重做外科AVR来管理失败的生物假体:在倾向匹配人群中的早期和晚期结果。
目的本研究的目的是比较重做外科主动脉瓣置换(AVR)和瓣膜内瓣膜导管(ViV)经导管AVR之间的早期和晚期结局。背景技术迄今为止,比较失败的生物假体的重做外科手术AVR(RS)与ViV经导管AVR的比较研究规模很小,并且仅限于早期结果。方法将加拿大人口最多的安大略省的临床和行政数据库链接起来,以获取因先前的生物修复失败而接受ViV和RS治疗的患者。进行倾向得分匹配以解决基线特征的差异。使用McNemar检验比较早期结果。使用Cox比例风险模型比较了匹配组之间的晚期死亡率。结果纳入2008年3月31日至2017年9月30日之间在安大略省的11家医疗机构(ViV,n = 214; RS,n = 344)进行的因生物假体失败而接受干预的558名患者。接受ViV的患者年龄较大,合并症更多。对27个变量的倾向匹配产生了相似的组进行比较(n = 131对)。从初始AVR到RS或ViV的平均时间分别为8.6±4.4年和11.3±4.5年。与RS相比,ViV的30天死亡率显着降低(绝对风险差异:-7.5%; 95%置信区间:-12.6%至-2.3%)。ViV的永久起搏器植入和输血率以及住院时间也较低。ViV的5年生存率更高(76.8%比66.8%;危险比:0.55; 95%置信区间:0.30至0.99; p = 0.04)。
更新日期:2020-01-15
中文翻译:

经导管ViV与重做外科AVR来管理失败的生物假体:在倾向匹配人群中的早期和晚期结果。
目的本研究的目的是比较重做外科主动脉瓣置换(AVR)和瓣膜内瓣膜导管(ViV)经导管AVR之间的早期和晚期结局。背景技术迄今为止,比较失败的生物假体的重做外科手术AVR(RS)与ViV经导管AVR的比较研究规模很小,并且仅限于早期结果。方法将加拿大人口最多的安大略省的临床和行政数据库链接起来,以获取因先前的生物修复失败而接受ViV和RS治疗的患者。进行倾向得分匹配以解决基线特征的差异。使用McNemar检验比较早期结果。使用Cox比例风险模型比较了匹配组之间的晚期死亡率。结果纳入2008年3月31日至2017年9月30日之间在安大略省的11家医疗机构(ViV,n = 214; RS,n = 344)进行的因生物假体失败而接受干预的558名患者。接受ViV的患者年龄较大,合并症更多。对27个变量的倾向匹配产生了相似的组进行比较(n = 131对)。从初始AVR到RS或ViV的平均时间分别为8.6±4.4年和11.3±4.5年。与RS相比,ViV的30天死亡率显着降低(绝对风险差异:-7.5%; 95%置信区间:-12.6%至-2.3%)。ViV的永久起搏器植入和输血率以及住院时间也较低。ViV的5年生存率更高(76.8%比66.8%;危险比:0.55; 95%置信区间:0.30至0.99; p = 0.04)。











































 京公网安备 11010802027423号
京公网安备 11010802027423号