Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Primary care physician knowledge, attitudes, and diagnostic testing practices for norovirus and acute gastroenteritis.
PLOS ONE ( IF 2.9 ) Pub Date : 2020-01-14 , DOI: 10.1371/journal.pone.0227890 Cristina V Cardemil 1 , Sean T O'Leary 2, 3 , Brenda L Beaty 2 , Katy Ivey 1 , Megan C Lindley 1 , Allison Kempe 2, 3 , Lori A Crane 2, 4 , Laura P Hurley 2, 5 , Michaela Brtnikova 2, 3 , Aron J Hall 1
PLOS ONE ( IF 2.9 ) Pub Date : 2020-01-14 , DOI: 10.1371/journal.pone.0227890 Cristina V Cardemil 1 , Sean T O'Leary 2, 3 , Brenda L Beaty 2 , Katy Ivey 1 , Megan C Lindley 1 , Allison Kempe 2, 3 , Lori A Crane 2, 4 , Laura P Hurley 2, 5 , Michaela Brtnikova 2, 3 , Aron J Hall 1
Affiliation
|
BACKGROUND
Norovirus is a leading cause of acute gastroenteritis (AGE) across the age spectrum; candidate vaccines are in clinical trials. While norovirus diagnostic testing is increasingly available, stool testing may not be performed routinely, which can hamper surveillance and burden of disease estimates. Additionally, lack of knowledge of the burden of disease may inhibit provider vaccine recommendations, which could affect coverage rates and ultimately the impact of the vaccine. Our objectives were to understand physicians' stool testing practices in outpatients with AGE, and physician knowledge of norovirus, in order to improve surveillance and prepare for vaccine introduction.
METHODS
Internet and mail survey on AGE, norovirus, and future norovirus vaccines conducted January to March 2018 among national networks of primary care pediatricians, family practice and general internal medicine physicians.
RESULTS
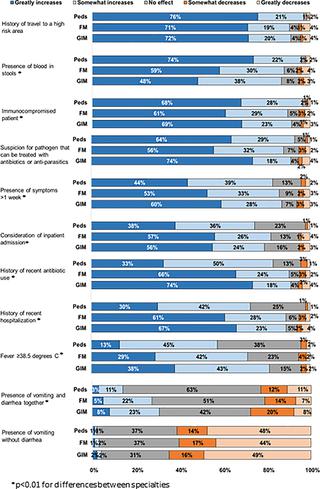
The response rate was 59% (820/1383). During peak AGE season, physicians estimated they ordered stool tests for a median of 15% (interquartile range: 5-33%) of their outpatients with AGE. Stool tests were reported as more often available for ova and parasites, Clostridioides difficile, and bacterial culture (>95% for all specialties) than for norovirus (6-33% across specialties); even when available, norovirus-specific tests were infrequently ordered. Most providers were unaware that norovirus is a leading cause of AGE across all age groups (Pediatricians 80%, Family Practice 86%, General Internal Medicine 89%) or that alcohol-based hand sanitizers are ineffective against norovirus (Pediatricians 51%, Family Practice 66%, General Internal Medicine 62%). Concerns cited as major barriers to implementing a future norovirus vaccine included if the vaccine is not covered by insurance (General Internal Medicine 64%, Pediatricians 67%, Family Practice 74%) and lack of adequate reimbursement for vaccination (Pediatricians 43%, General Internal Medicine 46%, Family Practice 50%). Factors that providers believed were 'not at all a barrier' or 'minor barrier' to new vaccine introduction included the belief that "my patients won't need this vaccine" (General Internal Medicine 78%, Family Practice 86%, Pediatricians 90%) and "my patients already get too many vaccines" (Family Practice 89%, General Internal Medicine 92%, Pediatricians 95%).
CONCLUSIONS
Primary care physicians had few concerns regarding future norovirus vaccine introduction, but have knowledge gaps on norovirus prevalence and hand hygiene for prevention. Also, physicians infrequently order stool tests for outpatients with AGE, which limits surveillance estimates that rely on physician-ordered stool diagnostics. Closing physician knowledge gaps on norovirus burden and transmission can help support norovirus vaccine introduction.
中文翻译:

初级保健医生对诺如病毒和急性胃肠炎的知识、态度和诊断测试实践。
背景诺如病毒是各个年龄段急性胃肠炎(AGE)的主要原因。候选疫苗正在进行临床试验。虽然诺如病毒诊断检测越来越多,但粪便检测可能不会常规进行,这可能会妨碍监测和疾病负担估计。此外,缺乏对疾病负担的了解可能会抑制提供者的疫苗推荐,这可能会影响覆盖率并最终影响疫苗的影响。我们的目标是了解医生对 AGE 门诊患者的粪便检测实践以及医生对诺如病毒的了解,以改善监测并为疫苗的引入做好准备。方法 2018 年 1 月至 3 月,在全国初级保健儿科医生、家庭医生和普通内科医生网络中进行了有关 AGE、诺如病毒和未来诺如病毒疫苗的互联网和邮件调查。结果 有效率 59% (820/1383)。在 AGE 高峰季节,医生估计他们对 AGE 门诊患者中中位数 15%(四分位距:5-33%)进行了粪便检查。据报道,粪便检测更常用于检测虫卵和寄生虫、艰难梭菌和细菌培养(所有专业的 95% 以上),而不是诺如病毒(所有专业的 6-33%);即使有诺如病毒特异性检测,也很少进行。大多数提供者不知道诺如病毒是所有年龄段 AGE 的主要原因(儿科医生 80%,家庭诊所 86%,普通内科 89%),或者酒精类洗手液对诺如病毒无效(儿科医生 51%,家庭诊所66%,普通内科 62%)。 被认为是实施未来诺如病毒疫苗的主要障碍的担忧包括疫苗是否不在保险范围内(普通内科 64%、儿科医生 67%、家庭诊所 74%)以及缺乏足够的疫苗接种报销(儿科医生 43%、普通内科)医学 46%,家庭医学 50%)。提供者认为引入新疫苗“根本不是障碍”或“次要障碍”的因素包括“我的患者不需要这种疫苗”的信念(普通内科 78%、家庭诊所 86%、儿科医生 90%) )和“我的患者已经接种了太多疫苗”(家庭诊所 89%,普通内科 92%,儿科医生 95%)。结论 初级保健医生对未来诺如病毒疫苗的引入几乎没有担忧,但在诺如病毒流行和预防手部卫生方面存在知识差距。此外,医生很少为 AGE 门诊患者安排粪便检测,这限制了依赖医生安排的粪便诊断的监测估计。缩小医生在诺如病毒负担和传播方面的知识差距可以帮助支持诺如病毒疫苗的引进。
更新日期:2020-01-15
中文翻译:

初级保健医生对诺如病毒和急性胃肠炎的知识、态度和诊断测试实践。
背景诺如病毒是各个年龄段急性胃肠炎(AGE)的主要原因。候选疫苗正在进行临床试验。虽然诺如病毒诊断检测越来越多,但粪便检测可能不会常规进行,这可能会妨碍监测和疾病负担估计。此外,缺乏对疾病负担的了解可能会抑制提供者的疫苗推荐,这可能会影响覆盖率并最终影响疫苗的影响。我们的目标是了解医生对 AGE 门诊患者的粪便检测实践以及医生对诺如病毒的了解,以改善监测并为疫苗的引入做好准备。方法 2018 年 1 月至 3 月,在全国初级保健儿科医生、家庭医生和普通内科医生网络中进行了有关 AGE、诺如病毒和未来诺如病毒疫苗的互联网和邮件调查。结果 有效率 59% (820/1383)。在 AGE 高峰季节,医生估计他们对 AGE 门诊患者中中位数 15%(四分位距:5-33%)进行了粪便检查。据报道,粪便检测更常用于检测虫卵和寄生虫、艰难梭菌和细菌培养(所有专业的 95% 以上),而不是诺如病毒(所有专业的 6-33%);即使有诺如病毒特异性检测,也很少进行。大多数提供者不知道诺如病毒是所有年龄段 AGE 的主要原因(儿科医生 80%,家庭诊所 86%,普通内科 89%),或者酒精类洗手液对诺如病毒无效(儿科医生 51%,家庭诊所66%,普通内科 62%)。 被认为是实施未来诺如病毒疫苗的主要障碍的担忧包括疫苗是否不在保险范围内(普通内科 64%、儿科医生 67%、家庭诊所 74%)以及缺乏足够的疫苗接种报销(儿科医生 43%、普通内科)医学 46%,家庭医学 50%)。提供者认为引入新疫苗“根本不是障碍”或“次要障碍”的因素包括“我的患者不需要这种疫苗”的信念(普通内科 78%、家庭诊所 86%、儿科医生 90%) )和“我的患者已经接种了太多疫苗”(家庭诊所 89%,普通内科 92%,儿科医生 95%)。结论 初级保健医生对未来诺如病毒疫苗的引入几乎没有担忧,但在诺如病毒流行和预防手部卫生方面存在知识差距。此外,医生很少为 AGE 门诊患者安排粪便检测,这限制了依赖医生安排的粪便诊断的监测估计。缩小医生在诺如病毒负担和传播方面的知识差距可以帮助支持诺如病毒疫苗的引进。











































 京公网安备 11010802027423号
京公网安备 11010802027423号