Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Patient-Reported Outcomes Through 5 Years for Active Surveillance, Surgery, Brachytherapy, or External Beam Radiation With or Without Androgen Deprivation Therapy for Localized Prostate Cancer
JAMA ( IF 63.1 ) Pub Date : 2020-01-14 , DOI: 10.1001/jama.2019.20675 Karen E Hoffman 1 , David F Penson 2 , Zhiguo Zhao 3 , Li-Ching Huang 3 , Ralph Conwill 4 , Aaron A Laviana 2 , Daniel D Joyce 2 , Amy N Luckenbaugh 2 , Michael Goodman 5 , Ann S Hamilton 6 , Xiao-Cheng Wu 7 , Lisa E Paddock 8 , Antoinette Stroup 8 , Matthew R Cooperberg 9 , Mia Hashibe 10 , Brock B O'Neil 11 , Sherrie H Kaplan 12 , Sheldon Greenfield 12 , Tatsuki Koyama 3 , Daniel A Barocas 2
JAMA ( IF 63.1 ) Pub Date : 2020-01-14 , DOI: 10.1001/jama.2019.20675 Karen E Hoffman 1 , David F Penson 2 , Zhiguo Zhao 3 , Li-Ching Huang 3 , Ralph Conwill 4 , Aaron A Laviana 2 , Daniel D Joyce 2 , Amy N Luckenbaugh 2 , Michael Goodman 5 , Ann S Hamilton 6 , Xiao-Cheng Wu 7 , Lisa E Paddock 8 , Antoinette Stroup 8 , Matthew R Cooperberg 9 , Mia Hashibe 10 , Brock B O'Neil 11 , Sherrie H Kaplan 12 , Sheldon Greenfield 12 , Tatsuki Koyama 3 , Daniel A Barocas 2
Affiliation
|
Importance
Understanding adverse effects of contemporary treatment approaches for men with favorable-risk and unfavorable-risk localized prostate cancer could inform treatment selection. Objective
To compare functional outcomes associated with prostate cancer treatments over 5 years after treatment. Design, Setting, and Participants
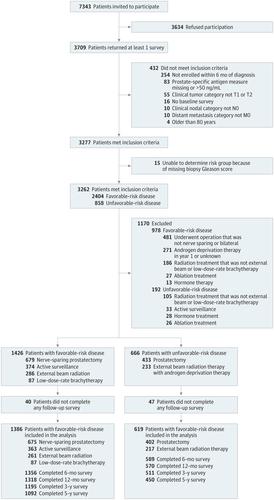
Prospective, population-based cohort study of 1386 men with favorable-risk (clinical stage cT1 to cT2bN0M0, prostate-specific antigen [PSA] ≤20 ng/mL, and Grade Group 1-2) prostate cancer and 619 men with unfavorable-risk (clinical stage cT2cN0M0, PSA of 20-50 ng/mL, or Grade Group 3-5) prostate cancer diagnosed in 2011 through 2012, accrued from 5 Surveillance, Epidemiology and End Results Program sites and a US prostate cancer registry, with surveys through September 2017. Exposures
Treatment with active surveillance (n = 363), nerve-sparing prostatectomy (n = 675), external beam radiation therapy (EBRT; n = 261), or low-dose-rate brachytherapy (n = 87) for men with favorable-risk disease and treatment with prostatectomy (n = 402) or EBRT with androgen deprivation therapy (n = 217) for men with unfavorable-risk disease. Main Outcomes and Measures
Patient-reported function, based on the 26-item Expanded Prostate Index Composite (range, 0-100), 5 years after treatment. Regression models were adjusted for baseline function and patient and tumor characteristics. Minimum clinically important difference was 10 to 12 for sexual function, 6 to 9 for urinary incontinence, 5 to 7 for urinary irritative symptoms, and 4 to 6 for bowel and hormonal function. Results
A total of 2005 men met inclusion criteria and completed the baseline and at least 1 postbaseline survey (median [interquartile range] age, 64 [59-70] years; 1529 of 1993 participants [77%] were non-Hispanic white). For men with favorable-risk prostate cancer, nerve-sparing prostatectomy was associated with worse urinary incontinence at 5 years (adjusted mean difference, -10.9 [95% CI, -14.2 to -7.6]) and sexual function at 3 years (adjusted mean difference, -15.2 [95% CI, -18.8 to -11.5]) compared with active surveillance. Low-dose-rate brachytherapy was associated with worse urinary irritative (adjusted mean difference, -7.0 [95% CI, -10.1 to -3.9]), sexual (adjusted mean difference, -10.1 [95% CI, -14.6 to -5.7]), and bowel (adjusted mean difference, -5.0 [95% CI, -7.6 to -2.4]) function at 1 year compared with active surveillance. EBRT was associated with urinary, sexual, and bowel function changes not clinically different from active surveillance at any time point through 5 years. For men with unfavorable-risk disease, EBRT with ADT was associated with lower hormonal function at 6 months (adjusted mean difference, -5.3 [95% CI, -8.2 to -2.4]) and bowel function at 1 year (adjusted mean difference, -4.1 [95% CI, -6.3 to -1.9]), but better sexual function at 5 years (adjusted mean difference, 12.5 [95% CI, 6.2-18.7]) and incontinence at each time point through 5 years (adjusted mean difference, 23.2 [95% CI, 17.7-28.7]), than prostatectomy. Conclusions and Relevance
In this cohort of men with localized prostate cancer, most functional differences associated with contemporary management options attenuated by 5 years. However, men undergoing prostatectomy reported clinically meaningful worse incontinence through 5 years compared with all other options, and men undergoing prostatectomy for unfavorable-risk disease reported worse sexual function at 5 years compared with men who underwent EBRT with ADT.
中文翻译:

患者报告的局部前列腺癌 5 年主动监测、手术、近距离放射治疗或外照射(联合或不联合雄激素剥夺疗法)的结果
重要性了解当代治疗方法对患有有利风险和不利风险局限性前列腺癌的男性的不利影响可以为治疗选择提供信息。目的 比较治疗后 5 年内与前列腺癌治疗相关的功能结果。设计、背景和参与者 对 1386 名患有有利风险(临床分期 cT1 至 cT2bN0M0、前列腺特异性抗原 [PSA] ≤ 20 ng/mL、等级组 1-2)前列腺癌和2011 年至 2012 年期间诊断出的 619 名患有不利风险(临床阶段 cT2cN0M0、PSA 为 20-50 ng/mL 或 3-5 级)前列腺癌的男性,来自 5 个监测、流行病学和最终结果计划站点和一个美国前列腺癌症登记处,调查截至 2017 年 9 月。 暴露 主动监测治疗 (n = 363)、保留神经的前列腺切除术 (n = 675)、外照射放射治疗 (EBRT;n = 261) 或低剂量率近距离放射治疗 (n = 261) n = 87) 对于患有有利风险疾病的男性,并采用前列腺切除术 (n = 402) 或 EBRT 联合雄激素剥夺疗法 (n = 217) 对患有不利风险疾病的男性进行治疗。主要结果和措施 治疗后 5 年患者报告的功能,基于 26 项综合前列腺扩张指数(范围,0-100)。根据基线功能以及患者和肿瘤特征调整回归模型。性功能的最小临床重要差异为 10 至 12,尿失禁为 6 至 9,尿路刺激症状为 5 至 7,肠道和激素功能为 4 至 6。 结果 共有 2005 名男性符合纳入标准,并完成了基线调查和至少 1 次基线后调查(中位[四分位距]年龄为 64 [59-70] 岁;1993 名参与者中有 1529 名 [77%] 为非西班牙裔白人)。对于患有高危前列腺癌的男性,保留神经的前列腺切除术与 5 年时更严重的尿失禁(调整后的平均差,-10.9 [95% CI,-14.2 至 -7.6])和 3 年时的性功能(调整后的平均差)相关。与主动监测相比,差异为-15.2 [95% CI,-18.8 至 -11.5])。低剂量率近距离放射治疗与更严重的尿路刺激性(调整后平均差,-7.0 [95% CI,-10.1 至 -3.9])、性(调整后平均差,-10.1 [95% CI,-14.6 至 -5.7])相关。 ]),与主动监测相比,1 年时肠功能(调整后平均差,-5.0 [95% CI,-7.6 至 -2.4])。 EBRT 与泌尿、性功能和肠道功能变化相关,在临床上与 5 年任何时间点的主动监测没有不同。对于患有不良风险疾病的男性,EBRT 联合 ADT 与 6 个月时较低的激素功能(调整后平均差,-5.3 [95% CI,-8.2 至 -2.4])和 1 年时肠功能较低(调整后平均差,-5.3 [95% CI,-8.2 至 -2.4])相关。 -4.1 [95% CI, -6.3 至 -1.9]),但 5 年时性功能更好(调整后平均差,12.5 [95% CI, 6.2-18.7]),并且 5 年内每个时间点都有失禁(调整后平均差)与前列腺切除术相比,差异为 23.2 [95% CI,17.7-28.7])。结论和相关性 在这组患有局限性前列腺癌的男性中,大多数与当代治疗方案相关的功能差异减弱了 5 年。 然而,与所有其他选择相比,接受前列腺切除术的男性在 5 年内报告了具有临床意义的更严重的尿失禁,并且与接受 EBRT 联合 ADT 的男性相比,因不良风险疾病而接受前列腺切除术的男性在 5 年后报告性功能更差。
更新日期:2020-01-14
中文翻译:

患者报告的局部前列腺癌 5 年主动监测、手术、近距离放射治疗或外照射(联合或不联合雄激素剥夺疗法)的结果
重要性了解当代治疗方法对患有有利风险和不利风险局限性前列腺癌的男性的不利影响可以为治疗选择提供信息。目的 比较治疗后 5 年内与前列腺癌治疗相关的功能结果。设计、背景和参与者 对 1386 名患有有利风险(临床分期 cT1 至 cT2bN0M0、前列腺特异性抗原 [PSA] ≤ 20 ng/mL、等级组 1-2)前列腺癌和2011 年至 2012 年期间诊断出的 619 名患有不利风险(临床阶段 cT2cN0M0、PSA 为 20-50 ng/mL 或 3-5 级)前列腺癌的男性,来自 5 个监测、流行病学和最终结果计划站点和一个美国前列腺癌症登记处,调查截至 2017 年 9 月。 暴露 主动监测治疗 (n = 363)、保留神经的前列腺切除术 (n = 675)、外照射放射治疗 (EBRT;n = 261) 或低剂量率近距离放射治疗 (n = 261) n = 87) 对于患有有利风险疾病的男性,并采用前列腺切除术 (n = 402) 或 EBRT 联合雄激素剥夺疗法 (n = 217) 对患有不利风险疾病的男性进行治疗。主要结果和措施 治疗后 5 年患者报告的功能,基于 26 项综合前列腺扩张指数(范围,0-100)。根据基线功能以及患者和肿瘤特征调整回归模型。性功能的最小临床重要差异为 10 至 12,尿失禁为 6 至 9,尿路刺激症状为 5 至 7,肠道和激素功能为 4 至 6。 结果 共有 2005 名男性符合纳入标准,并完成了基线调查和至少 1 次基线后调查(中位[四分位距]年龄为 64 [59-70] 岁;1993 名参与者中有 1529 名 [77%] 为非西班牙裔白人)。对于患有高危前列腺癌的男性,保留神经的前列腺切除术与 5 年时更严重的尿失禁(调整后的平均差,-10.9 [95% CI,-14.2 至 -7.6])和 3 年时的性功能(调整后的平均差)相关。与主动监测相比,差异为-15.2 [95% CI,-18.8 至 -11.5])。低剂量率近距离放射治疗与更严重的尿路刺激性(调整后平均差,-7.0 [95% CI,-10.1 至 -3.9])、性(调整后平均差,-10.1 [95% CI,-14.6 至 -5.7])相关。 ]),与主动监测相比,1 年时肠功能(调整后平均差,-5.0 [95% CI,-7.6 至 -2.4])。 EBRT 与泌尿、性功能和肠道功能变化相关,在临床上与 5 年任何时间点的主动监测没有不同。对于患有不良风险疾病的男性,EBRT 联合 ADT 与 6 个月时较低的激素功能(调整后平均差,-5.3 [95% CI,-8.2 至 -2.4])和 1 年时肠功能较低(调整后平均差,-5.3 [95% CI,-8.2 至 -2.4])相关。 -4.1 [95% CI, -6.3 至 -1.9]),但 5 年时性功能更好(调整后平均差,12.5 [95% CI, 6.2-18.7]),并且 5 年内每个时间点都有失禁(调整后平均差)与前列腺切除术相比,差异为 23.2 [95% CI,17.7-28.7])。结论和相关性 在这组患有局限性前列腺癌的男性中,大多数与当代治疗方案相关的功能差异减弱了 5 年。 然而,与所有其他选择相比,接受前列腺切除术的男性在 5 年内报告了具有临床意义的更严重的尿失禁,并且与接受 EBRT 联合 ADT 的男性相比,因不良风险疾病而接受前列腺切除术的男性在 5 年后报告性功能更差。











































 京公网安备 11010802027423号
京公网安备 11010802027423号