当前位置:
X-MOL 学术
›
Hypertens. Res.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
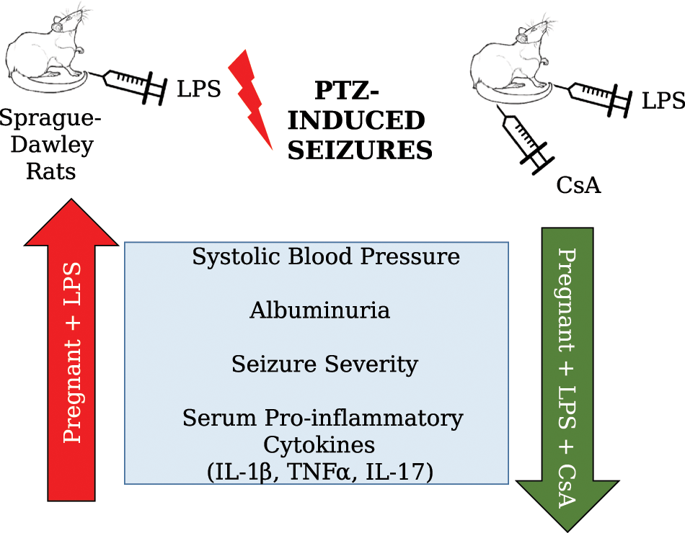
Targeting inflammation to reduce seizure severity in an experimental model of eclampsia
Hypertension Research ( IF 4.3 ) Pub Date : 2020-01-14 , DOI: 10.1038/s41440-019-0317-4 Frank T Spradley 1
Hypertension Research ( IF 4.3 ) Pub Date : 2020-01-14 , DOI: 10.1038/s41440-019-0317-4 Frank T Spradley 1
Affiliation
|
Eclampsia, which refers to new-onset seizures in pregnant women without a history of seizure disorder, is associated with high maternal and fetal morbidity and mortality. Most commonly, eclampsia occurs as a progression from preeclampsia (PE), a disorder of new-onset hypertension and cardiovascular, renal, visual, and brain disturbances in the latter half of pregnancy. The incidence rate of PE ranges from 2 to 5% in developed countries and up to 18% in parts of Africa [1]. If PE is severe enough and left untreated, neurological problems can result. The brain can be affected, resulting in abnormal cerebral vascular function, blood brain barrier leakage, and edema that can cause the convulsive seizures that define eclampsia; this can ultimately result in death from hemorrhagic stroke. The rate of eclampsia is ~0.05%, but can reach 0.8% in developing countries, and eclampsia contributes to 7% of maternal deaths and 18% of fetal deaths [2]. Therefore, research on this area of maternal health is important for identifying mechanistic targets that translate to cost-effective treatments for PE and eclampsia. Currently, magnesium sulfate (MgSO4) is the primary treatment and it is administered prophylactically to women with severe PE who are at risk of developing eclampsia. While MgSO4 is effective in preventing seizures, it is not as effective in reducing hypertension or proteinuria in PE patients. Thus, finding a therapeutic agent that improves multiple PE symptoms is necessary. This issue of Hypertension Research includes a study conducted by Huang et al. entitled ‘Cyclosporin A ameliorates eclampsia seizure through reducing systemic inflammation in an eclampsialike rat model’. By utilizing an experimental animal model, this study provides some important information about the mechanistic basis of the onset of eclamptic seizures. The purpose of this editorial is to summarize this original manuscript and to review the strengths and limitations of this study in which the authors examined the mechanisms that mediate the dangerous progression of PE to eclamptic seizures. PE and eclampsia develop suddenly in humans, but there are no experimental research models to date that spontaneously develop these maternal disorders. Thus, investigators rely upon pharmacological and/or surgical models. This study by Huang and colleagues used a model of PE generated by injecting an ultralow dose of lipopolysaccharide (LPS) endotoxin on gestational day 14 followed by the I.P. injection of pentylenetetrazol (PTZ, a GABA receptor antagonist) at the end of gestation on day 20 to induce seizures. This paradigm was based on previous studies by the investigators in which LPS-induced preeclamptic rats, compared with normal pregnant rats, exhibited increased susceptibility to PTZ-induced seizures. In addition, the authors showed in earlier studies that the LPS model of PE exhibits the shortest latency to develop PTZ-induced seizures, the longest seizure duration, and the highest recorded EEG amplitudes along with neuronal loss in the hippocampus [3]. Neuronal hyperactivity in this brain region is linked to the onset of seizures [4]. While the observed functional and morphological changes are associated with central and systemic inflammation, the previous studies did not examine whether the increased susceptibility to seizures is mediated by pro-inflammatory pathways. The novelty of the current study is that the authors examined the causative pathways, whereby PE increases the risk for eclampsia. The present study confirmed that LPS-induced preeclamptic rats have increased blood pressure (as determined by tail cuff plethysmography), albuminuria, seizure severity, and systemic inflammation by day 19/20 (Fig. 1). The pro-inflammatory markers included elevations in the levels of interleukin (IL)-1β, tumor necrosis factor (TNF)-α, and IL-17 in the circulation. To begin examining the role of pro-inflammatory pathways in mediating increased * Frank T. Spradley fspradley@gmail.com
更新日期:2020-01-14











































 京公网安备 11010802027423号
京公网安备 11010802027423号