American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2020-01-10 , DOI: 10.1053/j.ajkd.2019.09.016 Jeffrey Perl 1 , Douglas S Fuller 2 , Brian A Bieber 2 , Neil Boudville 3 , Talerngsak Kanjanabuch 4 , Yasuhiko Ito 5 , Sharon J Nessim 6 , Beth M Piraino 7 , Ronald L Pisoni 2 , Bruce M Robinson 2 , Douglas E Schaubel 8 , Martin J Schreiber 9 , Isaac Teitelbaum 10 , Graham Woodrow 11 , Junhui Zhao 2 , David W Johnson 12
|
Rationale & Objective
Peritoneal dialysis (PD)-related peritonitis carries high morbidity for PD patients. Understanding the characteristics and risk factors for peritonitis can guide regional development of prevention strategies. We describe peritonitis rates and the associations of selected facility practices with peritonitis risk among countries participating in the Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS).
Study Design
Observational prospective cohort study.
Setting & Participants
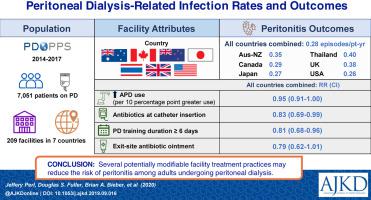
7,051 adult PD patients in 209 facilities across 7 countries (Australia, New Zealand, Canada, Japan, Thailand, United Kingdom, United States).
Exposures
Facility characteristics (census count, facility age, nurse to patient ratio) and selected facility practices (use of automated PD, use of icodextrin or biocompatible PD solutions, antibiotic prophylaxis strategies, duration of PD training).
Outcomes
Peritonitis rate (by country, overall and variation across facilities), microbiology patterns.
Analytical Approach
Poisson rate estimation, proportional rate models adjusted for selected patient case-mix variables.
Results
2,272 peritonitis episodes were identified in 7,051 patients (crude rate, 0.28 episodes/patient-year). Facility peritonitis rates were variable within each country and exceeded 0.50/patient-year in 10% of facilities. Overall peritonitis rates, in episodes per patient-year, were 0.40 (95% CI, 0.36-0.46) in Thailand, 0.38 (95% CI, 0.32-0.46) in the United Kingdom, 0.35 (95% CI, 0.30-0.40) in Australia/New Zealand, 0.29 (95% CI, 0.26-0.32) in Canada, 0.27 (95% CI, 0.25-0.30) in Japan, and 0.26 (95% CI, 0.24-0.27) in the United States. The microbiology of peritonitis was similar across countries, except in Thailand, where Gram-negative infections and culture-negative peritonitis were more common. Facility size was positively associated with risk for peritonitis in Japan (rate ratio [RR] per 10 patients, 1.07; 95% CI, 1.04-1.09). Lower peritonitis risk was observed in facilities that had higher automated PD use (RR per 10 percentage points greater, 0.95; 95% CI, 0.91-1.00), facilities that used antibiotics at catheter insertion (RR, 0.83; 95% CI, 0.69-0.99), and facilities with PD training duration of 6 or more (vs <6) days (RR, 0.81; 95% CI, 0.68-0.96). Lower peritonitis risk was seen in facilities that used topical exit-site mupirocin or aminoglycoside ointment, but this association did not achieve conventional levels of statistical significance (RR, 0.79; 95% CI, 0.62-1.01).
Limitations
Sampling variation, selection bias (rate estimates), and residual confounding (associations).
Conclusions
Important international differences exist in the risk for peritonitis that may result from varied and potentially modifiable treatment practices. These findings may inform future guidelines in potentially setting lower maximally acceptable peritonitis rates.
中文翻译:

腹膜透析相关的感染率和结果:腹膜透析结果和实践模式研究(PDOPPS)的结果。
理由与目标
腹膜透析(PD)相关的腹膜炎对PD患者的发病率很高。了解腹膜炎的特征和危险因素可以指导预防策略的区域发展。我们描述了参与腹膜透析结果和实践模式研究(PDOPPS)的国家之间的腹膜炎发生率以及所选设施实践与腹膜炎风险之间的关联。
学习规划
观察性前瞻性队列研究。
设置与参与者
在7个国家(澳大利亚,新西兰,加拿大,日本,泰国,英国,美国)的209家机构中,有7,051名成人PD患者。
曝光量
设施特征(人口普查,设施年龄,护士与患者的比例)和选定的设施实践(使用自动PD,使用艾考糊精或生物相容性PD解决方案,抗生素预防策略,PD培训时间)。
结果
腹膜炎发生率(按国家,总体和设施的不同而变化),微生物学模式。
分析方法
泊松比率估计,针对选定的患者病例混合变量调整比例比率模型。
结果
在7,051名患者中发现了2,272例腹膜炎发作(粗暴率,0.28例/患者/年)。每个国家/地区的设施腹膜炎发生率各不相同,在10%的设施中,每位患者每年超过0.50。在每个患者年的发作中,总体腹膜炎发生率在泰国为0.40(95%CI,0.36-0.46),在英国为0.38(95%CI,0.32-0.46),0.35(95%CI,0.30-0.40)澳大利亚/新西兰,加拿大的0.29(95%CI,0.26-0.32),日本的0.27(95%CI,0.25-0.30)和美国的0.26(95%CI,0.24-0.27)。除了泰国以外,其他国家的腹膜炎的微生物学相似,除了泰国,革兰氏阴性感染和培养阴性的腹膜炎更为常见。在日本,机构规模与腹膜炎风险呈正相关(每10例患者的比率[RR]为1.07; 95%CI为1.04-1.09)。在具有较高自动PD使用量的设施(RR比每升高10个百分点,0.95; 95%CI,0.91-1.00),在导管插入时使用抗生素的设施(RR,0.83; 95%CI,0.69- 0.99),以及PD训练时间为6天或以上(vs <6)天的设施(RR,0.81; 95%CI,0.68-0.96)。在使用局部出口部位莫匹罗星或氨基糖苷软膏的医疗机构中,发现腹膜炎的风险较低,但这种关联并未达到常规的统计学显着水平(RR,0.79; 95%CI,0.62-1.01)。0.68-0.96)。在使用局部出口部位莫匹罗星或氨基糖苷软膏的医疗机构中,发现腹膜炎的风险较低,但这种关联并未达到常规的统计学显着水平(RR,0.79; 95%CI,0.62-1.01)。0.68-0.96)。在使用局部出口部位莫匹罗星或氨基糖苷软膏的医疗机构中,发现腹膜炎的风险较低,但这种关联并未达到常规的统计学显着水平(RR,0.79; 95%CI,0.62-1.01)。
局限性
抽样变异,选择偏差(估计率)和残留混杂(关联)。
结论
腹膜炎的风险在国际上存在重要差异,这种差异可能是由于治疗方法的不同和潜在的可修改性造成的。这些发现可能会为将来的指南提供指导,以潜在地降低最大可接受腹膜炎的发生率。











































 京公网安备 11010802027423号
京公网安备 11010802027423号