当前位置:
X-MOL 学术
›
JAMA Oncol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association Between 21-Gene Assay Recurrence Score and Locoregional Recurrence Rates in Patients With Node-Positive Breast Cancer.
JAMA Oncology ( IF 22.5 ) Pub Date : 2020-01-09 , DOI: 10.1001/jamaoncol.2019.5559 Wendy A Woodward 1 , William E Barlow 2 , Reshma Jagsi 3 , Thomas A Buchholz 1 , Steven Shak 4 , Frederick Baehner 4, 5 , Timothy J Whelan 6 , Nancy E Davidson 7, 8 , James N Ingle 9 , Tari A King 10 , Peter M Ravdin 11 , C Kent Osborne 12 , Debasish Tripathy 13 , Robert B Livingston 14 , Julie R Gralow 15 , Gabriel N Hortobagyi 13 , Daniel F Hayes 16 , Kathy S Albain 17
JAMA Oncology ( IF 22.5 ) Pub Date : 2020-01-09 , DOI: 10.1001/jamaoncol.2019.5559 Wendy A Woodward 1 , William E Barlow 2 , Reshma Jagsi 3 , Thomas A Buchholz 1 , Steven Shak 4 , Frederick Baehner 4, 5 , Timothy J Whelan 6 , Nancy E Davidson 7, 8 , James N Ingle 9 , Tari A King 10 , Peter M Ravdin 11 , C Kent Osborne 12 , Debasish Tripathy 13 , Robert B Livingston 14 , Julie R Gralow 15 , Gabriel N Hortobagyi 13 , Daniel F Hayes 16 , Kathy S Albain 17
Affiliation
|
Importance
The 21-gene assay recurrence score is increasingly used to personalize treatment recommendations for systemic therapy in postmenopausal women with estrogen receptor (ER)- or progesterone receptor (PR)-positive, node-positive breast cancer; however, the relevance of the 21-gene assay to radiotherapy decisions remains uncertain.
Objective
To examine the association between recurrence score and locoregional recurrence (LRR) in a postmenopausal patient population treated with adjuvant chemotherapy followed by tamoxifen or tamoxifen alone.
Design, Setting, and Participants
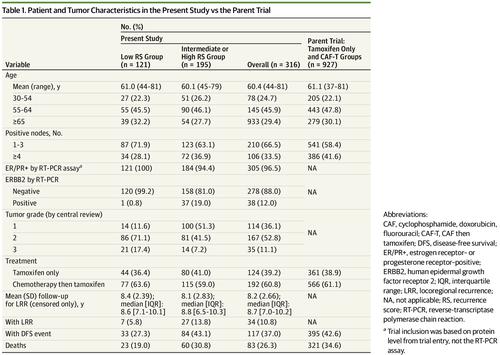
This cohort study was a retrospective analysis of the Southwest Oncology Group S8814, a phase 3 randomized clinical trial of postmenopausal women with ER/PR-positive, node-positive breast cancer treated with tamoxifen alone, chemotherapy followed by tamoxifen, or concurrent tamoxifen and chemotherapy. Patients at North American clinical centers were enrolled from June 1989 to July 1995. Medical records from patients with recurrence score information were reviewed for LRR and radiotherapy use. Primary analysis included 316 patients and excluded 37 who received both mastectomy and radiotherapy, 9 who received breast-conserving surgery without documented radiotherapy, and 5 with unknown surgical type. All analyses were performed from January 22, 2016, to August 9, 2019.
Main Outcomes and Measures
The LRR was defined as a recurrence in the breast; chest wall; or axillary, infraclavicular, supraclavicular, or internal mammary lymph nodes. Time to LRR was tested with log-rank tests and Cox proportional hazards regression for multivariate models.
Results
The final cohort of this study comprised 316 women with a mean (range) age of 60.4 (44-81) years. Median (interquartile range) follow-up for those without LRR was 8.7 (7.0-10.2) years. Seven LRR events (5.8%) among 121 patients with low recurrence score and 27 LRR events (13.8%) among 195 patients with intermediate or high recurrence score occurred. The estimated 10-year cumulative incidence rates were 9.7% for those with a low recurrence score and 16.5% for the group with intermediate or high recurrence score (P = .02). Among patients who had a mastectomy without radiotherapy (n = 252), the differences in the 10-year actuarial LRR rates remained significant: 7.7 % for the low recurrence score group vs 16.8% for the intermediate or high recurrence score group (P = .03). A multivariable model controlling for randomized treatment, number of positive nodes, and surgical type showed that a higher recurrence score was prognostic for LRR (hazard ratio [HR], 2.36; 95% CI, 1.02-5.45; P = .04). In a subset analysis of patients with a mastectomy and 1 to 3 involved nodes who did not receive radiation therapy, the group with a low recurrence score had a 1.5% rate of LRR, whereas the group with an intermediate or high recurrence score had a 11.1% LRR (P = .051).
Conclusions and Relevance
This study found that higher recurrence scores were associated with increased LRR after adjustment for treatment, type of surgical procedure, and number of positive nodes. This finding suggests that the recurrence score may be used, along with accepted clinical variables, to assess the risk of LRR during radiotherapy decision-making.
中文翻译:

淋巴结阳性乳腺癌患者的21基因检测复发评分与局部复发率之间的关联。
重要性21基因测定的复发评分越来越多地用于个性化治疗建议,用于绝经后雌激素受体(ER)或孕激素受体(PR)阳性,淋巴结阳性乳腺癌的女性;然而,21基因检测与放射治疗决策的相关性仍不确定。目的探讨绝经后接受辅助化疗,他莫昔芬或他莫昔芬治疗的绝经后患者人群中复发评分与局部复发(LRR)之间的关系。设计,背景和参与者这项队列研究是对西南肿瘤学S8814组的回顾性分析,该组是ER / PR阳性,淋巴结阳性的绝经后妇女单独接受他莫昔芬治疗,化疗及他莫昔芬治疗的3期随机临床试验。 ,或并发他莫昔芬和化疗。1989年6月至1995年7月在北美临床中心登记的患者入组。对具有复发评分信息的患者的病历进行了LRR和放疗的使用进行了审查。初步分析包括316例患者,其中37例同时接受了乳房切除术和放射治疗,9例接受了保乳手术而没有记录的放射治疗,5例手术类型不明。所有分析均于2016年1月22日至2019年8月9日进行。主要结果和措施LRR的定义是乳房复发。胸壁 或腋窝,锁骨下,锁骨上或内部乳腺淋巴结。LRR时间用对数秩检验和Cox比例风险回归进行多变量模型测试。结果本研究的最后一个队列包括316名女性(平均(年龄)年龄为60.4(44-81)岁)。没有LRR的患者的中位(四分位间距)随访时间为8.7(7.0-10.2)年。在121例低复发评分患者中发生了7例LRR事件(5.8%),在195例中度或高复发评分患者中发生了27例LRR事件(13.8%)。低复发评分者的十年累计发病率估计为9.7%,中,高复发评分者为16.5%(P = .02)。在未经放射治疗的乳房切除术患者中(n = 252),十年期精算LRR率的差异仍然很明显:低复发评分组为7.7%,中或高复发评分组为16.8%(P =。 03)。控制随机治疗的多变量模型,阳性淋巴结数目和手术类型表明,LRR的复发评分更高(危险比[HR]为2.36; 95%CI为1.02-5.45; P = .04)。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。手术类型显示LRR的复发分数更高(危险比[HR]为2.36; 95%CI为1.02-5.45; P = .04)。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。手术类型显示LRR的复发分数更高(危险比[HR]为2.36; 95%CI为1.02-5.45; P = .04)。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。而中度或高复发评分组的LRR为11.1%(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。而中度或高复发评分组的LRR为11.1%(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。
更新日期:2020-04-01
中文翻译:

淋巴结阳性乳腺癌患者的21基因检测复发评分与局部复发率之间的关联。
重要性21基因测定的复发评分越来越多地用于个性化治疗建议,用于绝经后雌激素受体(ER)或孕激素受体(PR)阳性,淋巴结阳性乳腺癌的女性;然而,21基因检测与放射治疗决策的相关性仍不确定。目的探讨绝经后接受辅助化疗,他莫昔芬或他莫昔芬治疗的绝经后患者人群中复发评分与局部复发(LRR)之间的关系。设计,背景和参与者这项队列研究是对西南肿瘤学S8814组的回顾性分析,该组是ER / PR阳性,淋巴结阳性的绝经后妇女单独接受他莫昔芬治疗,化疗及他莫昔芬治疗的3期随机临床试验。 ,或并发他莫昔芬和化疗。1989年6月至1995年7月在北美临床中心登记的患者入组。对具有复发评分信息的患者的病历进行了LRR和放疗的使用进行了审查。初步分析包括316例患者,其中37例同时接受了乳房切除术和放射治疗,9例接受了保乳手术而没有记录的放射治疗,5例手术类型不明。所有分析均于2016年1月22日至2019年8月9日进行。主要结果和措施LRR的定义是乳房复发。胸壁 或腋窝,锁骨下,锁骨上或内部乳腺淋巴结。LRR时间用对数秩检验和Cox比例风险回归进行多变量模型测试。结果本研究的最后一个队列包括316名女性(平均(年龄)年龄为60.4(44-81)岁)。没有LRR的患者的中位(四分位间距)随访时间为8.7(7.0-10.2)年。在121例低复发评分患者中发生了7例LRR事件(5.8%),在195例中度或高复发评分患者中发生了27例LRR事件(13.8%)。低复发评分者的十年累计发病率估计为9.7%,中,高复发评分者为16.5%(P = .02)。在未经放射治疗的乳房切除术患者中(n = 252),十年期精算LRR率的差异仍然很明显:低复发评分组为7.7%,中或高复发评分组为16.8%(P =。 03)。控制随机治疗的多变量模型,阳性淋巴结数目和手术类型表明,LRR的复发评分更高(危险比[HR]为2.36; 95%CI为1.02-5.45; P = .04)。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。手术类型显示LRR的复发分数更高(危险比[HR]为2.36; 95%CI为1.02-5.45; P = .04)。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。手术类型显示LRR的复发分数更高(危险比[HR]为2.36; 95%CI为1.02-5.45; P = .04)。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。在对未接受放射治疗的乳房切除术和1至3个受累淋巴结的患者进行的子集分析中,复发评分低的组的LRR率为1.5%,而复发评分中等或高的组的11.1。 %LRR(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。而中度或高复发评分组的LRR为11.1%(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。而中度或高复发评分组的LRR为11.1%(P = .051)。结论与相关性本研究发现,较高的复发分数与调整治疗,手术方法和阳性淋巴结数目后的LRR增加有关。这一发现表明,可以将复发评分与公认的临床变量一起用于评估放疗决策过程中LRR的风险。











































 京公网安备 11010802027423号
京公网安备 11010802027423号