当前位置:
X-MOL 学术
›
JACC Heart Fail.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Mineralocorticoid Receptor Antagonists, Blood Pressure, and Outcomes in Heart Failure With Reduced Ejection Fraction.
JACC: Heart Failure ( IF 13.0 ) Pub Date : 2020-01-06 , DOI: 10.1016/j.jchf.2019.09.011 Matteo Serenelli 1 , Alice Jackson 2 , Pooja Dewan 2 , Pardeep S Jhund 2 , Mark C Petrie 2 , Patrick Rossignol 3 , Gianluca Campo 4 , Bertram Pitt 5 , Faiez Zannad 3 , João Pedro Ferreira 6 , John J V McMurray 2
JACC: Heart Failure ( IF 13.0 ) Pub Date : 2020-01-06 , DOI: 10.1016/j.jchf.2019.09.011 Matteo Serenelli 1 , Alice Jackson 2 , Pooja Dewan 2 , Pardeep S Jhund 2 , Mark C Petrie 2 , Patrick Rossignol 3 , Gianluca Campo 4 , Bertram Pitt 5 , Faiez Zannad 3 , João Pedro Ferreira 6 , John J V McMurray 2
Affiliation
|
OBJECTIVES
The purpose of this study was to investigate the effects of mineralocorticoid receptor antagonists (MRAs) on systolic blood pressure (SBP) and outcomes according to baseline SBP in patients with heart failure with reduced ejection fraction (HFrEF).
BACKGROUND
MRAs are greatly underused in patients with HFrEF, often because of fear of adverse events. Concern about hypotension has been raised by the demonstration that MRAs are particularly effective treatment for resistant hypertension.
METHODS
The effect of MRA therapy was studied in 4,396 patients with HFrEF randomized in the RALES (Randomized Aldactone Evaluation Study) and EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure) trials.
RESULTS
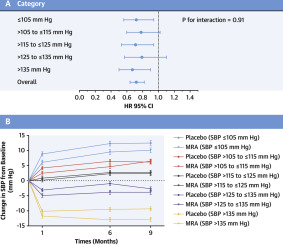
Mean SBP change from baseline to 6 months was +1.4 ± 18.1 mm Hg in the placebo group and -1.2 ± 17.9 mm Hg in the MRA group. The between-treatment difference was 2.6 (95% confidence interval [CI]: 1.5 to 3.6; p < 0.001) mm Hg. All outcomes were reduced by MRA therapy overall, with consistent effects across SBP categories (e.g., all-cause mortality, overall hazard ratio [HR] of 0.72; 95% CI: 0.64 to 0.82; p < 0.001; SBP ≤105 mm Hg; HR: 0.72; 95% CI: 0.56 to 0.94; SBP >105 to ≤115 mm Hg; HR: 0.78; 95% CI: 0.60 to 1.02; SBP >115 to ≤125 mm Hg; HR: 0.71; 95% CI: 0.53 to 0.94; SBP >125 to ≤135 mm Hg; HR: 0.79; 95% CI: 0.57 to 1.10; and SBP > 135 mm Hg; HR: 0.67; 95% CI: 0.50 to 0.90; p for interaction = 0.95). Hypotension was infrequent and not more common with MRA therapy than with placebo, overall (4.6% vs. 3.9%; p = 0.25) or in any SBP category.
CONCLUSIONS
MRA treatment had little effect on SBP in patients with HFrEF, and the clinical benefits were not modified by baseline SBP. MRA treatment infrequently caused hypotension, even when the baseline SBP was low. The treatment discontinuation rates between MRA and placebo therapy were similar. Low SBP is not a reason to withhold MRA therapy in patients with HFrEF.
中文翻译:

盐皮质激素受体拮抗剂,血压和射血分数降低的心力衰竭结果。
目的本研究的目的是根据射血分数降低(HFrEF)的心力衰竭患者,研究盐皮质激素受体拮抗剂(MRA)对收缩压(SBP)和预后的影响。背景技术经常由于担心不良事件而在HFrEF患者中未充分使用MRA。通过证明MRA对抵抗性高血压特别有效的治疗,引起了人们对低血压的担忧。方法在随机研究的4 396例HFrEF患者中研究了MRA治疗的效果,该患者随机进行了RALES(随机分组的Aldactone评估研究)和EMPHASIS-HF(轻度患者住院治疗中的依普利酮和心衰生存研究)试验。结果安慰剂组从基线到6个月的平均SBP变化为+1.4±18.1 mm Hg,-1.2±17。MRA组中为9毫米汞柱。治疗之间的差异为2.6毫米汞柱(95%置信区间[CI]:1.5至3.6; p <0.001)。总体而言,MRA治疗降低了所有结局,并且在SBP类别之间具有一致的效果(例如,全因死亡率,总危险比[HR]为0.72; 95%CI:0.64至0.82; p <0.001; SBP≤105mm Hg; SBP≤105mm Hg; P <0.001)。 HR:0.72; 95%CI:0.56至0.94; SBP> 105至≤115mm Hg; HR:0.78; 95%CI:0.60至1.02; SBP> 115至≤125mm Hg; HR:0.71; 95%CI: 0.53至0.94; SBP> 125至≤135mm Hg; HR:0.79; 95%CI:0.57至1.10; SBP> 135 mm Hg; HR:0.67; 95%CI:0.50至0.90;相互作用的p = 0.95) 。低血压并不常见,在MRA治疗中总的来说(4.6%vs. 3.9%; p = 0.25)或任何SBP类别中的高血压患者都不多。结论MRA治疗对HFrEF患者的SBP影响不大,并且基线SBP并未改变临床获益。即使基线SBP较低,MRA治疗也很少引起低血压。MRA和安慰剂治疗之间的治疗终止率相似。低SBP并不是在HFrEF患者中停止MRA治疗的原因。
更新日期:2020-01-09
中文翻译:

盐皮质激素受体拮抗剂,血压和射血分数降低的心力衰竭结果。
目的本研究的目的是根据射血分数降低(HFrEF)的心力衰竭患者,研究盐皮质激素受体拮抗剂(MRA)对收缩压(SBP)和预后的影响。背景技术经常由于担心不良事件而在HFrEF患者中未充分使用MRA。通过证明MRA对抵抗性高血压特别有效的治疗,引起了人们对低血压的担忧。方法在随机研究的4 396例HFrEF患者中研究了MRA治疗的效果,该患者随机进行了RALES(随机分组的Aldactone评估研究)和EMPHASIS-HF(轻度患者住院治疗中的依普利酮和心衰生存研究)试验。结果安慰剂组从基线到6个月的平均SBP变化为+1.4±18.1 mm Hg,-1.2±17。MRA组中为9毫米汞柱。治疗之间的差异为2.6毫米汞柱(95%置信区间[CI]:1.5至3.6; p <0.001)。总体而言,MRA治疗降低了所有结局,并且在SBP类别之间具有一致的效果(例如,全因死亡率,总危险比[HR]为0.72; 95%CI:0.64至0.82; p <0.001; SBP≤105mm Hg; SBP≤105mm Hg; P <0.001)。 HR:0.72; 95%CI:0.56至0.94; SBP> 105至≤115mm Hg; HR:0.78; 95%CI:0.60至1.02; SBP> 115至≤125mm Hg; HR:0.71; 95%CI: 0.53至0.94; SBP> 125至≤135mm Hg; HR:0.79; 95%CI:0.57至1.10; SBP> 135 mm Hg; HR:0.67; 95%CI:0.50至0.90;相互作用的p = 0.95) 。低血压并不常见,在MRA治疗中总的来说(4.6%vs. 3.9%; p = 0.25)或任何SBP类别中的高血压患者都不多。结论MRA治疗对HFrEF患者的SBP影响不大,并且基线SBP并未改变临床获益。即使基线SBP较低,MRA治疗也很少引起低血压。MRA和安慰剂治疗之间的治疗终止率相似。低SBP并不是在HFrEF患者中停止MRA治疗的原因。



























 京公网安备 11010802027423号
京公网安备 11010802027423号