当前位置:
X-MOL 学术
›
JAMA Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Comparison of Decompressing Stoma vs Stent as a Bridge to Surgery for Left-Sided Obstructive Colon Cancer.
JAMA Surgery ( IF 15.7 ) Pub Date : 2020-01-08 , DOI: 10.1001/jamasurg.2019.5466 Joyce V Veld 1, 2 , Femke J Amelung 3 , Wernard A A Borstlap 1 , Emo E van Halsema 2 , Esther C J Consten 3, 4 , Peter D Siersema 5 , Frank Ter Borg 6 , Edwin S van der Zaag 7 , Johannes H W de Wilt 8 , Paul Fockens 2 , Wilhelmus A Bemelman 1 , Jeanin E van Hooft 2 , Pieter J Tanis 1 ,
JAMA Surgery ( IF 15.7 ) Pub Date : 2020-01-08 , DOI: 10.1001/jamasurg.2019.5466 Joyce V Veld 1, 2 , Femke J Amelung 3 , Wernard A A Borstlap 1 , Emo E van Halsema 2 , Esther C J Consten 3, 4 , Peter D Siersema 5 , Frank Ter Borg 6 , Edwin S van der Zaag 7 , Johannes H W de Wilt 8 , Paul Fockens 2 , Wilhelmus A Bemelman 1 , Jeanin E van Hooft 2 , Pieter J Tanis 1 ,
Affiliation
|
Importance
Bridge to elective surgery using self-expandable metal stent (SEMS) placement is a debated alternative to emergency resection for patients with left-sided obstructive colon cancer because of oncologic concerns. A decompressing stoma (DS) might be a valid alternative, but relevant studies are scarce.
Objective
To compare DS with SEMS as a bridge to surgery for nonlocally advanced left-sided obstructive colon cancer using propensity score matching.
Design, Setting, and Participants
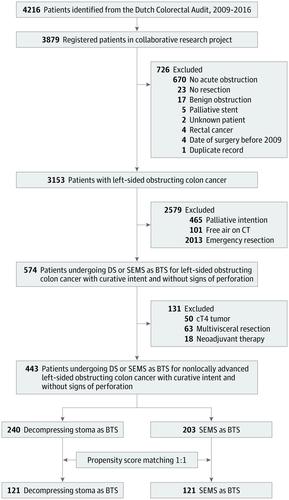
This national, population-based cohort study was performed at 75 of 77 hospitals in the Netherlands. A total of 4216 patients with left-sided obstructive colon cancer treated from January 1, 2009, to December 31, 2016, were identified from the Dutch Colorectal Audit and 3153 patients were studied. Additional procedural and intermediate-term outcome data were retrospectively collected from individual patient files, resulting in a median follow-up of 32 months (interquartile range, 15-57 months). Data were analyzed from April 7 to October 28, 2019.
Exposures
Decompressing stoma vs SEMS as a bridge to surgery.
Main Outcomes and Measures
Primary anastomosis rate, postresection presence of a stoma, complications, additional interventions, permanent stoma, locoregional recurrence, disease-free survival, and overall survival. Propensity score matching was performed according to age, sex, body mass index, American Society of Anesthesiologists score, prior abdominal surgery, tumor location, pN stage, cM stage, length of stenosis, and year of resection.
Results
A total of 3153 of the eligible 4216 patients were included in the study (mean [SD] age, 69.7 [11.8] years; 1741 [55.2%] male); after exclusions, 443 patients underwent bridge to surgery (240 undergoing DS and 203 undergoing SEMS). Propensity score matching led to 2 groups of 121 patients each. Patients undergoing SEMS had more primary anastomoses (104 of 121 [86.0%] vs 90 of 120 [75.0%], P = .02), more postresection stomas (81 of 121 [66.9%] vs 34 of 117 [29.1%], P < .001), fewer major complications (7 of 121 [5.8%] vs 18 of 118 [15.3%], P = .02), and more subsequent interventions, including stoma reversal (65 of 113 [57.5%] vs 33 of 117 [28.2%], P < .001). After DS and SEMS, the 3-year locoregional recurrence rates were 11.7% for DS and 18.8% for SEMS (hazard ratio [HR], 0.62; 95% CI, 0.30-1.28; P = .20), the 3-year disease-free survival rates were 64.0% for DS and 56.9% for SEMS (HR, 0.90; 95% CI, 0.61-1.33; P = .60), and the 3-year overall survival rates were 78.0% for DS and 71.8% for SEMS (HR, 0.77; 95% CI, 0.48-1.22; P = .26).
Conclusions and Relevance
The findings suggest that DS as bridge to resection of left-sided obstructive colon cancer is associated with advantages and disadvantages compared with SEMS, with similar intermediate-term oncologic outcomes. The existing equipoise indicates the need for a randomized clinical trial that compares the 2 bridging techniques.
中文翻译:

减压造口术与支架术的比较-左侧阻塞性结肠癌手术的桥梁。
对于自闭症左侧阻塞性结肠癌患者而言,由于肿瘤学原因,使用自膨胀金属支架(SEMS)放置择期手术的重要性是急诊切除术的替代方案。减压造口术(DS)可能是有效的替代方法,但相关研究很少。目的比较倾向评分匹配技术将DS与SEMS作为非局部晚期左侧阻塞性结肠癌手术的桥梁。设计,设置和参与者这项全国性的队列研究是在荷兰的77家医院中的75家进行的。从2009年1月1日至2016年12月31日,从荷兰大肠直肠癌审核中心(Dutch Check)总共鉴定了4216例左侧阻塞性结肠癌患者,并研究了3153例患者。回顾性地从个别患者档案中收集了其他程序和中期结局数据,平均随访32个月(四分位间距为15-57个月)。从2019年4月7日至10月28日对数据进行了分析。暴露减压造口vs SEMS是通向手术的桥梁。主要结果和措施主要吻合率,切除后是否存在造口,并发症,其他干预措施,永久性造口,局部复发,无病生存和总体生存。根据年龄,性别,体重指数,美国麻醉医师学会评分,先前的腹部手术,肿瘤位置,pN分期,cM分期,狭窄时间和切除年限进行倾向得分匹配。结果纳入研究的4216例患者中,共有3153例(平均[SD]年龄,69.7 [11.8]岁; 1741 [55.2%]男性);排除后,有443例患者接受了手术治疗(240例行DS和203例行SEMS)。倾向得分匹配导致两组,每组121位患者。接受SEMS的患者有更多的原发性吻合术(121例中的104例[86.0%]比120例中的90例[75.0%],P = .02),切除后的气孔更多(121例中81例[66.9%]比117例中的34例[29.1%], P <.001),主要并发症更少(121例中的7例[5.8%]比118例中的18例[15.3%],P = .02)以及更多的后续干预措施,包括造口逆转(65例中113例[57.5%]对比33例) 117 [28.2%],P <.001)。在进行DS和SEMS后,DS的3年局部复发率和SEMS的3年局部复发率(危险比[HR]为0.62; 95%CI为0.30-1.28; P = 0.20),DS的3年无病生存率和SEMS的3年无病生存率(HR,0.90; 95%CI,0.61-1.33; P = .60),3年的总生存率为78.0% DS和SEMS占71.8%(HR,0.77; 95%CI,0.48-1.22; P = 0.26)。结论与相关性研究结果表明,与SEMS相比,DS作为切除左侧阻塞性结肠癌的桥梁具有优缺点,中期肿瘤学预后相似。现有的设备表明需要比较两种桥接技术的随机临床试验。结论与相关性研究结果表明,与SEMS相比,DS作为切除左侧阻塞性结肠癌的桥梁具有优缺点,中期肿瘤学预后相似。现有的设备表明需要比较两种桥接技术的随机临床试验。结论与相关性研究结果表明,与SEMS相比,DS作为切除左侧阻塞性结肠癌的桥梁具有优缺点,中期肿瘤学预后相似。现有的设备表明需要比较两种桥接技术的随机临床试验。
更新日期:2020-03-19
中文翻译:

减压造口术与支架术的比较-左侧阻塞性结肠癌手术的桥梁。
对于自闭症左侧阻塞性结肠癌患者而言,由于肿瘤学原因,使用自膨胀金属支架(SEMS)放置择期手术的重要性是急诊切除术的替代方案。减压造口术(DS)可能是有效的替代方法,但相关研究很少。目的比较倾向评分匹配技术将DS与SEMS作为非局部晚期左侧阻塞性结肠癌手术的桥梁。设计,设置和参与者这项全国性的队列研究是在荷兰的77家医院中的75家进行的。从2009年1月1日至2016年12月31日,从荷兰大肠直肠癌审核中心(Dutch Check)总共鉴定了4216例左侧阻塞性结肠癌患者,并研究了3153例患者。回顾性地从个别患者档案中收集了其他程序和中期结局数据,平均随访32个月(四分位间距为15-57个月)。从2019年4月7日至10月28日对数据进行了分析。暴露减压造口vs SEMS是通向手术的桥梁。主要结果和措施主要吻合率,切除后是否存在造口,并发症,其他干预措施,永久性造口,局部复发,无病生存和总体生存。根据年龄,性别,体重指数,美国麻醉医师学会评分,先前的腹部手术,肿瘤位置,pN分期,cM分期,狭窄时间和切除年限进行倾向得分匹配。结果纳入研究的4216例患者中,共有3153例(平均[SD]年龄,69.7 [11.8]岁; 1741 [55.2%]男性);排除后,有443例患者接受了手术治疗(240例行DS和203例行SEMS)。倾向得分匹配导致两组,每组121位患者。接受SEMS的患者有更多的原发性吻合术(121例中的104例[86.0%]比120例中的90例[75.0%],P = .02),切除后的气孔更多(121例中81例[66.9%]比117例中的34例[29.1%], P <.001),主要并发症更少(121例中的7例[5.8%]比118例中的18例[15.3%],P = .02)以及更多的后续干预措施,包括造口逆转(65例中113例[57.5%]对比33例) 117 [28.2%],P <.001)。在进行DS和SEMS后,DS的3年局部复发率和SEMS的3年局部复发率(危险比[HR]为0.62; 95%CI为0.30-1.28; P = 0.20),DS的3年无病生存率和SEMS的3年无病生存率(HR,0.90; 95%CI,0.61-1.33; P = .60),3年的总生存率为78.0% DS和SEMS占71.8%(HR,0.77; 95%CI,0.48-1.22; P = 0.26)。结论与相关性研究结果表明,与SEMS相比,DS作为切除左侧阻塞性结肠癌的桥梁具有优缺点,中期肿瘤学预后相似。现有的设备表明需要比较两种桥接技术的随机临床试验。结论与相关性研究结果表明,与SEMS相比,DS作为切除左侧阻塞性结肠癌的桥梁具有优缺点,中期肿瘤学预后相似。现有的设备表明需要比较两种桥接技术的随机临床试验。结论与相关性研究结果表明,与SEMS相比,DS作为切除左侧阻塞性结肠癌的桥梁具有优缺点,中期肿瘤学预后相似。现有的设备表明需要比较两种桥接技术的随机临床试验。











































 京公网安备 11010802027423号
京公网安备 11010802027423号