当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Diastolic Blood Pressure and Heart Rate Are Independently Associated With Mortality in Chronic Aortic Regurgitation
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-01-01 , DOI: 10.1016/j.jacc.2019.10.047 Li-Tan Yang 1 , Patricia A Pellikka 1 , Maurice Enriquez-Sarano 1 , Christopher G Scott 2 , Ratnasari Padang 1 , Sunil V Mankad 1 , Hartzell V Schaff 3 , Hector I Michelena 1
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-01-01 , DOI: 10.1016/j.jacc.2019.10.047 Li-Tan Yang 1 , Patricia A Pellikka 1 , Maurice Enriquez-Sarano 1 , Christopher G Scott 2 , Ratnasari Padang 1 , Sunil V Mankad 1 , Hartzell V Schaff 3 , Hector I Michelena 1
Affiliation
|
BACKGROUND
The prognostic significance of diastolic blood pressure (DBP) and resting heart rate (RHR) in patients with hemodynamically significant aortic regurgitation (AR) is unknown. OBJECTIVES
This study sought to investigate the association of DBP and RHR with all-cause mortality in patients with AR. METHODS
Consecutive patients with ≥ moderate to severe AR were retrospectively identified from 2006 to 2017. The association between all-cause mortality and routinely measured DBP and RHR was examined. RESULTS
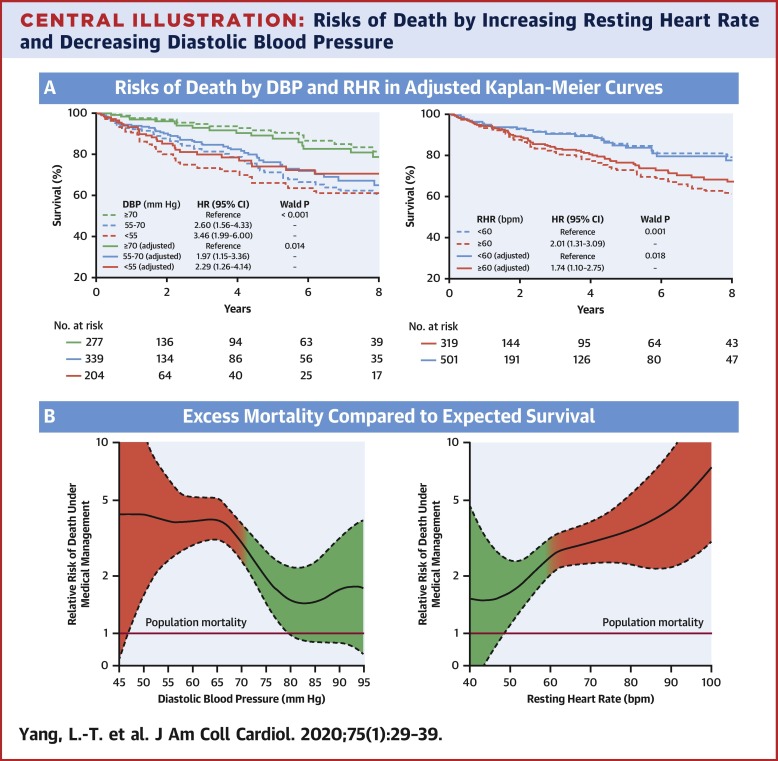
Of 820 patients (age 59 ± 17 years; 82% men) followed for 5.5 ± 3.5 years, 104 died under medical management, and 400 underwent aortic valve surgery (AVS). Age, symptoms, left ventricular ejection fraction (LVEF), LV end-systolic diameter-index (LVESDi), DBP, and RHR were univariable predictors of all-cause mortality (all p ≤ 0.002). When adjusted for demographics, comorbidities, and surgical triggers (symptoms, LVEF, and LVESDi), baseline DBP (adjusted-hazard ratio [HR]: 0.79 [95% confidence interval: 0.66 to 0.94] per 10 mm Hg increase, p = 0.009) and baseline RHR (adjusted HR: 1.23 [95% confidence interval: 1.03 to 1.45] per 10 beat per min [bpm] increase, p = 0.01) were independently associated with all-cause mortality. These associations persisted after adjustment for presence of hypertension, medications, time-dependent AVS, and using average DBP and RHR (all p ≤ 0.02). Compared with the general population, patients with AR exhibited excess mortality (relative risk of death >1), which rose steeply in inverse proportion (p nonlinearity = 0.002) to DBP starting at 70 mm Hg and peaking at 55 mm Hg and in direct proportion to RHR starting at 60 bpm. CONCLUSIONS
In patients with chronic hemodynamically significant AR, routinely measured DBP and RHR demonstrate a robust association with all-cause death, independent of demographics, comorbidities, guideline-based surgical triggers, presence of hypertension, and use of medications. Therefore, DBP and RHR should be integrated into comprehensive clinical decision-making for these patients.
中文翻译:

舒张压和心率与慢性主动脉瓣关闭不全的死亡率独立相关
背景 舒张压 (DBP) 和静息心率 (RHR) 对血流动力学显着的主动脉瓣关闭不全 (AR) 患者的预后意义尚不清楚。目的 本研究旨在调查 DBP 和 RHR 与 AR 患者全因死亡率的关系。方法 对 2006 年至 2017 年间连续发生≥中度至重度 AR 的患者进行回顾性鉴定。研究了全因死亡率与常规测量的 DBP 和 RHR 之间的关联。结果 在 820 名患者(年龄 59 ± 17 岁;82% 男性)中随访了 5.5 ± 3.5 年,104 人在医疗管理下死亡,400 人接受了主动脉瓣手术 (AVS)。年龄、症状、左心室射血分数 (LVEF)、左室收缩末期直径指数 (LVESDi)、DBP 和 RHR 是全因死亡率的单变量预测因子(所有 p ≤ 0.002)。当针对人口统计学、合并症和手术触发因素(症状、LVEF 和 LVESDi)进行调整后,基线 DBP(调整后的风险比 [HR]:0.79 [95% 置信区间:0.66 至 0.94]每增加 10 mmHg,p = 0.009 ) 和基线 RHR(调整后的 HR:1.23 [95% 置信区间:1.03 至 1.45] 每分钟 [bpm] 增加 10 次,p = 0.01)与全因死亡率独立相关。在调整高血压、药物、时间依赖性 AVS 并使用平均 DBP 和 RHR(所有 p ≤ 0.02)后,这些关联仍然存在。与一般人群相比,AR 患者表现出高死亡率(死亡相对风险 >1),与 DBP 成反比(p 非线性 = 0.002)急剧上升,从 70 mmHg 开始,在 55 mmHg 时达到峰值,并成正比从 60 bpm 开始到 RHR。结论 在慢性血流动力学显着 AR 患者中,常规测量的 DBP 和 RHR 表明与全因死亡密切相关,独立于人口统计学、合并症、基于指南的手术触发因素、高血压的存在和药物的使用。因此,应将 DBP 和 RHR 纳入这些患者的综合临床决策中。
更新日期:2020-01-01
中文翻译:

舒张压和心率与慢性主动脉瓣关闭不全的死亡率独立相关
背景 舒张压 (DBP) 和静息心率 (RHR) 对血流动力学显着的主动脉瓣关闭不全 (AR) 患者的预后意义尚不清楚。目的 本研究旨在调查 DBP 和 RHR 与 AR 患者全因死亡率的关系。方法 对 2006 年至 2017 年间连续发生≥中度至重度 AR 的患者进行回顾性鉴定。研究了全因死亡率与常规测量的 DBP 和 RHR 之间的关联。结果 在 820 名患者(年龄 59 ± 17 岁;82% 男性)中随访了 5.5 ± 3.5 年,104 人在医疗管理下死亡,400 人接受了主动脉瓣手术 (AVS)。年龄、症状、左心室射血分数 (LVEF)、左室收缩末期直径指数 (LVESDi)、DBP 和 RHR 是全因死亡率的单变量预测因子(所有 p ≤ 0.002)。当针对人口统计学、合并症和手术触发因素(症状、LVEF 和 LVESDi)进行调整后,基线 DBP(调整后的风险比 [HR]:0.79 [95% 置信区间:0.66 至 0.94]每增加 10 mmHg,p = 0.009 ) 和基线 RHR(调整后的 HR:1.23 [95% 置信区间:1.03 至 1.45] 每分钟 [bpm] 增加 10 次,p = 0.01)与全因死亡率独立相关。在调整高血压、药物、时间依赖性 AVS 并使用平均 DBP 和 RHR(所有 p ≤ 0.02)后,这些关联仍然存在。与一般人群相比,AR 患者表现出高死亡率(死亡相对风险 >1),与 DBP 成反比(p 非线性 = 0.002)急剧上升,从 70 mmHg 开始,在 55 mmHg 时达到峰值,并成正比从 60 bpm 开始到 RHR。结论 在慢性血流动力学显着 AR 患者中,常规测量的 DBP 和 RHR 表明与全因死亡密切相关,独立于人口统计学、合并症、基于指南的手术触发因素、高血压的存在和药物的使用。因此,应将 DBP 和 RHR 纳入这些患者的综合临床决策中。











































 京公网安备 11010802027423号
京公网安备 11010802027423号