当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Professional Dissonance and Burnout in Primary Care
JAMA Internal Medicine ( IF 39.0 ) Pub Date : 2020-03-01 , DOI: 10.1001/jamainternmed.2019.6326 Sumit D Agarwal 1, 2 , Erika Pabo 1, 2, 3 , Ronen Rozenblum 1, 2 , Karen M Sherritt 1, 2
JAMA Internal Medicine ( IF 39.0 ) Pub Date : 2020-03-01 , DOI: 10.1001/jamainternmed.2019.6326 Sumit D Agarwal 1, 2 , Erika Pabo 1, 2, 3 , Ronen Rozenblum 1, 2 , Karen M Sherritt 1, 2
Affiliation
|
Importance
Burnout negatively affects physician health, productivity, and patient care. Its prevalence is high among physicians, especially those in primary care, yet few qualitative studies of burnout have been performed that engage frontline primary care practitioners (PCPs) for their perspectives. Objective
To identify factors contributing to burnout and low professional fulfillment, as well as potential solutions, by eliciting the views of PCPs. Design, Setting, and Participants
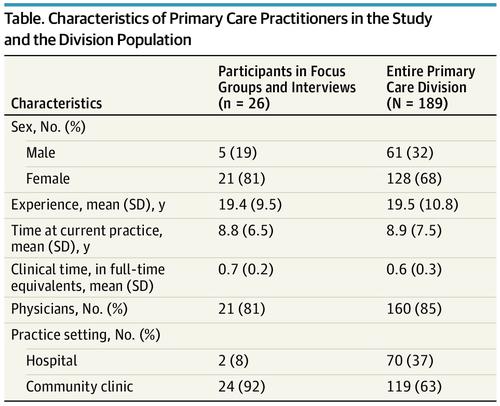
For this qualitative study, focus group discussions and interviews were conducted between February 1 and April 30, 2018, among 26 PCPs (physicians, nurse practitioners, and physician assistants) at a US academic medical center with a network of 15 primary care clinics. Participants were asked about factors contributing to burnout and barriers to professional fulfillment as well as potential solutions related to workplace culture and efficiency, work-life balance, and resilience. Main Outcomes and Measures
Perceptions of the factors contributing to burnout and low professional fulfillment as well as potential solutions. Results
A total of 26 PCPs (21 physicians, 3 nurse practitioners, and 2 physician assistants; 21 [81%] women) from 10 primary care clinics participated. They had a mean (SD) of 19.4 (9.5) years of clinical experience. Six common themes emerged from PCPs' experiences with burnout: 3 external contributing factors and 3 internal manifestations. Participants described their workloads as excessively heavy, increasingly involving less "doctor" work and more "office" work, and reflecting unreasonable expectations. They felt demoralized by work conditions, undervalued by local institutions and the health care system, and conflicted in their daily work. Participants conveyed a sense of professional dissonance, or discomfort from working in a system that seems to hold values counter to their values as clinicians. They suggested potential solutions clustered around 8 themes: managing the workload, caring for PCPs as multidimensional human beings, disconnecting from work, recalibrating expectations and reimbursement levels, promoting PCPs' voice, supporting professionalism, fostering community, and advocating reforms beyond the institution. Conclusions and Relevance
In sharing their perspectives on factors contributing to burnout, frontline PCPs interviewed during this study described dissonance between their professional values and the realities of primary care practice, an authority-responsibility mismatch, and a sense of undervaluation. Practitioners also identified possible solutions institutions might consider investing in to resolve professional dissonance, reduce burnout rates, and improve professional fulfillment.
中文翻译:

初级保健中的专业失调和倦怠
重要性倦怠会对医生的健康、工作效率和患者护理产生负面影响。它在医生中的流行率很高,尤其是在初级保健医生中,但很少有关于职业倦怠的定性研究让一线初级保健从业者 (PCP) 提出他们的观点。目标 通过征求 PCP 的意见,确定导致职业倦怠和职业成就感低下的因素以及潜在的解决方案。设计、设置和参与者 对于这项定性研究,焦点小组讨论和访谈是在 2018 年 2 月 1 日至 4 月 30 日期间在美国学术医疗中心的 26 名 PCP(医师、执业护士和医师助理)中进行的15个初级保健诊所。参与者被问及导致职业倦怠和障碍的因素,以及与工作场所文化和效率、工作与生活平衡以及适应能力相关的潜在解决方案。主要结果和措施 对导致职业倦怠和职业成就感低下的因素以及潜在解决方案的看法。结果 共有来自 10 个初级保健诊所的 26 名 PCP(21 名医师、3 名执业护士和 2 名医师助理;21 名 [81%] 女性)参与了研究。他们的临床经验平均 (SD) 为 19.4 (9.5) 年。PCP 的职业倦怠经历中出现了六个共同主题:3 个外部促成因素和 3 个内部表现。参与者形容他们的工作量过大,越来越少的“医生”工作和更多的“办公室”工作,并反映不合理的期望。他们对工作条件感到士气低落,被当地机构和医疗保健系统低估,并在日常工作中发生冲突。参与者传达了一种职业不协调感,或在一个似乎持有与他们作为临床医生的价值观背道而驰的系统中工作的不适感。他们提出了围绕 8 个主题的潜在解决方案:管理工作量、将 PCP 视为多维人、与工作脱节、重新调整期望和报销水平、促进 PCP 的声音、支持专业精神、培育社区以及倡导机构以外的改革。结论和相关性 在分享他们对导致倦怠的因素的看法时,在本研究中接受采访的一线 PCP 描述了他们的专业价值观与初级保健实践的现实之间的不一致、权威-责任不匹配以及被低估的感觉。从业者还确定了机构可能考虑投资以解决专业失调、降低职业倦怠率和提高专业成就感的可能解决方案。
更新日期:2020-03-01
中文翻译:

初级保健中的专业失调和倦怠
重要性倦怠会对医生的健康、工作效率和患者护理产生负面影响。它在医生中的流行率很高,尤其是在初级保健医生中,但很少有关于职业倦怠的定性研究让一线初级保健从业者 (PCP) 提出他们的观点。目标 通过征求 PCP 的意见,确定导致职业倦怠和职业成就感低下的因素以及潜在的解决方案。设计、设置和参与者 对于这项定性研究,焦点小组讨论和访谈是在 2018 年 2 月 1 日至 4 月 30 日期间在美国学术医疗中心的 26 名 PCP(医师、执业护士和医师助理)中进行的15个初级保健诊所。参与者被问及导致职业倦怠和障碍的因素,以及与工作场所文化和效率、工作与生活平衡以及适应能力相关的潜在解决方案。主要结果和措施 对导致职业倦怠和职业成就感低下的因素以及潜在解决方案的看法。结果 共有来自 10 个初级保健诊所的 26 名 PCP(21 名医师、3 名执业护士和 2 名医师助理;21 名 [81%] 女性)参与了研究。他们的临床经验平均 (SD) 为 19.4 (9.5) 年。PCP 的职业倦怠经历中出现了六个共同主题:3 个外部促成因素和 3 个内部表现。参与者形容他们的工作量过大,越来越少的“医生”工作和更多的“办公室”工作,并反映不合理的期望。他们对工作条件感到士气低落,被当地机构和医疗保健系统低估,并在日常工作中发生冲突。参与者传达了一种职业不协调感,或在一个似乎持有与他们作为临床医生的价值观背道而驰的系统中工作的不适感。他们提出了围绕 8 个主题的潜在解决方案:管理工作量、将 PCP 视为多维人、与工作脱节、重新调整期望和报销水平、促进 PCP 的声音、支持专业精神、培育社区以及倡导机构以外的改革。结论和相关性 在分享他们对导致倦怠的因素的看法时,在本研究中接受采访的一线 PCP 描述了他们的专业价值观与初级保健实践的现实之间的不一致、权威-责任不匹配以及被低估的感觉。从业者还确定了机构可能考虑投资以解决专业失调、降低职业倦怠率和提高专业成就感的可能解决方案。



























 京公网安备 11010802027423号
京公网安备 11010802027423号