当前位置:
X-MOL 学术
›
Modern Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Pathological assessment of endoscopic resections of the gastrointestinal tract: a comprehensive clinicopathologic review.
Modern Pathology ( IF 7.1 ) Pub Date : 2020-01-06 , DOI: 10.1038/s41379-019-0443-1 M Priyanthi Kumarasinghe 1 , Michael J Bourke 2 , Ian Brown 3, 4 , Peter V Draganov 5 , Duncan McLeod 6 , Catherine Streutker 7 , Spiro Raftopoulos 8 , Tetsuo Ushiku 9 , Gregory Y Lauwers 10
Modern Pathology ( IF 7.1 ) Pub Date : 2020-01-06 , DOI: 10.1038/s41379-019-0443-1 M Priyanthi Kumarasinghe 1 , Michael J Bourke 2 , Ian Brown 3, 4 , Peter V Draganov 5 , Duncan McLeod 6 , Catherine Streutker 7 , Spiro Raftopoulos 8 , Tetsuo Ushiku 9 , Gregory Y Lauwers 10
Affiliation
|
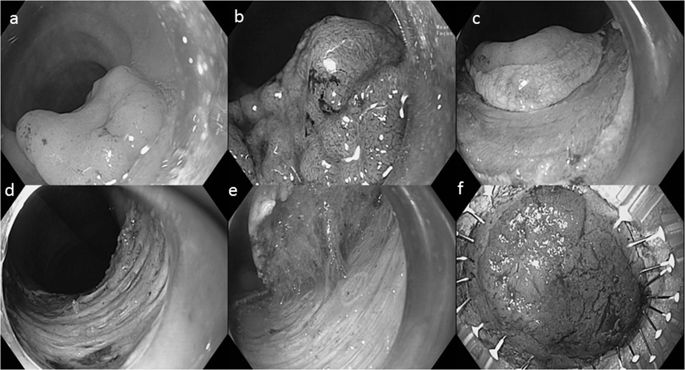
Endoscopic resection (ER) allows optimal staging with potential cure of early-stage luminal malignancies while maintaining organ preservation. ER and surgery are non-competing but complementary therapeutic options. In addition, histological examination of ER specimens can either confirm or refine the pre-procedure diagnosis. ER is used for the treatment of Barrett's related early carcinomas and dysplasias, early-esophageal squamous cell carcinomas and dysplasias, early gastric carcinomas and dysplasia, as well as low-risk submucosal invasive carcinomas (LR-SMIC) and, large laterally spreading adenomas of the colon. For invasive lesions, histological risk factors predict risk of lymph node metastasis and residual disease at the ER site. Important pathological risk factors predictive of lymph node metastasis are depth of tumor invasion, poor differentiation, and lymphovascular invasion. Complete resection with negative margins is critical to avoid local recurrences. For non-invasive lesions, complete resection is curative. Therefore, a systematic approach for handling and assessing ER specimens is recommended to evaluate all above key prognostic features appropriately. Correct handling starts with pinning the specimen before fixation, meticulous macroscopic assessment with orientation of appropriate margins, systematic sectioning, and microscopic assessment of the entire specimen. Microscopic examination should be thorough for accurate assessment of all pathological risk factors and margin assessment. Site-specific issues such as duplication of muscularis mucosa of the esophagus, challenges of assessing ampullectomy specimens and site-specific differences of staging of early carcinomas throughout the gastrointestinal tract (GI) tract should be given special consideration. Finally, a standard, comprehensive pathology report that allows optimal staging with potential cure of early-stage malignancies or better stratification and guidance for additional treatment should be provided.
中文翻译:

胃肠道内窥镜切除术的病理学评估:全面的临床病理学回顾。
内镜下切除术 (ER) 可实现最佳分期,并可能治愈早期管腔恶性肿瘤,同时保持器官保存。ER 和手术是非竞争性但互补的治疗选择。此外,ER 标本的组织学检查可以确认或改进术前诊断。ER 用于治疗 Barrett 相关的早期癌和异型增生、早期食管鳞状细胞癌和异型增生、早期胃癌和异型增生,以及低风险粘膜下浸润性癌 (LR-SMIC) 和大的横向扩散腺瘤冒号。对于侵袭性病变,组织学风险因素可预测 ER 部位淋巴结转移和残留病灶的风险。预测淋巴结转移的重要病理学危险因素是肿瘤浸润深度、分化差,淋巴血管浸润。完全切除且切缘阴性对于避免局部复发至关重要。对于非侵入性病变,完全切除是治愈性的。因此,建议采用系统的方法来处理和评估 ER 标本,以适当地评估上述所有关键预后特征。正确处理始于在固定前固定标本、细致的宏观评估以及适当边缘的定位、系统切片和整个标本的微观评估。显微镜检查应彻底,以准确评估所有病理危险因素和边缘评估。特定部位的问题,例如食管粘膜肌层重复,应特别考虑评估壶腹切除术标本的挑战以及整个胃肠道 (GI) 道早期癌分期的部位特异性差异。最后,应提供一份标准、全面的病理报告,以便对早期恶性肿瘤进行可能治愈的最佳分期或更好的分层和额外治疗指导。
更新日期:2020-01-06
中文翻译:

胃肠道内窥镜切除术的病理学评估:全面的临床病理学回顾。
内镜下切除术 (ER) 可实现最佳分期,并可能治愈早期管腔恶性肿瘤,同时保持器官保存。ER 和手术是非竞争性但互补的治疗选择。此外,ER 标本的组织学检查可以确认或改进术前诊断。ER 用于治疗 Barrett 相关的早期癌和异型增生、早期食管鳞状细胞癌和异型增生、早期胃癌和异型增生,以及低风险粘膜下浸润性癌 (LR-SMIC) 和大的横向扩散腺瘤冒号。对于侵袭性病变,组织学风险因素可预测 ER 部位淋巴结转移和残留病灶的风险。预测淋巴结转移的重要病理学危险因素是肿瘤浸润深度、分化差,淋巴血管浸润。完全切除且切缘阴性对于避免局部复发至关重要。对于非侵入性病变,完全切除是治愈性的。因此,建议采用系统的方法来处理和评估 ER 标本,以适当地评估上述所有关键预后特征。正确处理始于在固定前固定标本、细致的宏观评估以及适当边缘的定位、系统切片和整个标本的微观评估。显微镜检查应彻底,以准确评估所有病理危险因素和边缘评估。特定部位的问题,例如食管粘膜肌层重复,应特别考虑评估壶腹切除术标本的挑战以及整个胃肠道 (GI) 道早期癌分期的部位特异性差异。最后,应提供一份标准、全面的病理报告,以便对早期恶性肿瘤进行可能治愈的最佳分期或更好的分层和额外治疗指导。











































 京公网安备 11010802027423号
京公网安备 11010802027423号