当前位置:
X-MOL 学术
›
Prostate Cancer Prostatic. Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Clinicopathologic features and outcomes of anterior-dominant prostate cancer: implications for diagnosis and treatment.
Prostate Cancer and Prostatic Diseases ( IF 5.1 ) Pub Date : 2020-01-03 , DOI: 10.1038/s41391-019-0199-1 Sara M Falzarano 1 , Yaw A Nyame 2 , Jesse K McKenney 3, 4 , Christopher G Przybycin 3, 4 , Jianbo Li 5 , Andrew Stephenson 4 , Amr Fergany 4 , Ming Zhou 6 , Eric A Klein 4 , Cristina Magi-Galluzzi 7
Prostate Cancer and Prostatic Diseases ( IF 5.1 ) Pub Date : 2020-01-03 , DOI: 10.1038/s41391-019-0199-1 Sara M Falzarano 1 , Yaw A Nyame 2 , Jesse K McKenney 3, 4 , Christopher G Przybycin 3, 4 , Jianbo Li 5 , Andrew Stephenson 4 , Amr Fergany 4 , Ming Zhou 6 , Eric A Klein 4 , Cristina Magi-Galluzzi 7
Affiliation
|
OBJECTIVE
This study aims to describe the pathological features and clinical outcomes in anterior-dominant prostate cancer (APCA) compared to posterior/posterolateral-dominant prostate cancer (PPCA) among men treated with radical prostatectomy for localized prostate cancer.
METHODS
This is a single-institution, matched case-control analysis of short-term clinical outcomes stratified by pathologic tumor location at radical prostatectomy. Pathologic data extracted by expert genitourinary pathologists on tumor location was linked to clinical and oncologic outcomes data from a prospective institutional database for analysis.
RESULTS
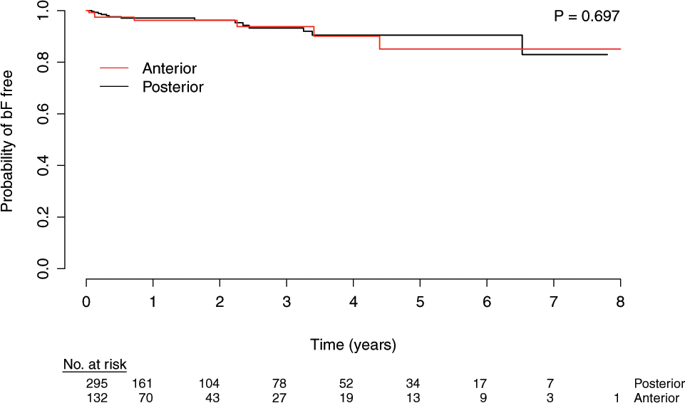
From 2005 to 2013, 1580 patients were identified for analysis with 150 (9.5%) having APCA. One-hundred and thirty two of these APCA men had complete clinical data and were matched to 353 men with PPCA (~1:3 ratio) by GrdGrp at surgery, margin status, and pathologic T stage. There were no racial/ethnic differences between APCA and PPCA (p = 0.13). Men with APCA demonstrated a higher median PSA at diagnosis (6.4 [4.6-9.1] ng/mL vs 5.6 [4.4-8.1] ng/mL; p = 0.04), a higher rate of GrdGrp 1 disease at diagnosis (57.7% vs. 40.0%, p = 0.003), and lower rates of abnormal digital rectal examination (DRE) (10.1% vs. 23.2%, p = 0.003) when compared to PPCA. The rate of surgical upgrading was higher among men with APCA vs. PPCA (55.3% vs 42.0%, p = 0.015). Freedom from biochemical failure (BF) at 5-years was 85.1% (95% CI 73.1-98.9) for APCA and 82.9% (95% CI 69.2-99.5) for men with PPCA (p = 0.70, log-rank test).
CONCLUSIONS
The majority of anterior tumors were undetectable by DRE and were associated with higher PSA at diagnosis. Despite presenting mostly as low/intermediate grade cancers, more than half of the men with APCA had upgrading at surgery and slightly more than 40% had positive margins and/or extraprostatic disease. When matched to a cohort of posterior predominant tumors, no differences were seen in the rate of biochemical-failure after prostatectomy.
中文翻译:

前优势前列腺癌的临床病理特征和结果:对诊断和治疗的影响。
目的 本研究旨在描述在接受根治性前列腺切除术治疗局限性前列腺癌的男性中,与后/后外侧优势前列腺癌 (PPCA) 相比,前优势前列腺癌 (APCA) 的病理特征和临床结果。方法 这是一项单一机构、匹配的病例对照分析,对根据根治性前列腺切除术的病理肿瘤位置分层的短期临床结果进行分析。由专家泌尿生殖病理学家提取的关于肿瘤位置的病理数据与来自前瞻性机构数据库的临床和肿瘤结果数据相关联以进行分析。结果 从 2005 年到 2013 年,确定了 1580 名患者进行分析,其中 150 名 (9.5%) 患有 APCA。这些 APCA 男性中有 132 名拥有完整的临床数据,并与 353 名患有 PPCA 的男性相匹配(~1:3 比率)通过手术、切缘状态和病理 T 分期的 GrdGrp。APCA 和 PPCA 之间没有种族/民族差异(p = 0.13)。患有 APCA 的男性在诊断时表现出较高的 PSA 中值(6.4 [4.6-9.1] ng/mL vs 5.6 [4.4-8.1] ng/mL;p = 0.04),诊断时 GrdGrp 1 疾病发生率更高(57.7% vs. 40.0%,p = 0.003),与 PPCA 相比,直肠指检 (DRE) 异常率较低(10.1% 对 23.2%,p = 0.003)。与 PPCA 相比,APCA 男性的手术升级率更高(55.3% 对 42.0%,p = 0.015)。APCA 的 5 年无生化失败 (BF) 率为 85.1% (95% CI 73.1-98.9),患有 PPCA 的男性为 82.9% (95% CI 69.2-99.5)(p = 0.70,对数秩检验)。结论 大多数前部肿瘤无法通过 DRE 检测到,并且与诊断时较高的 PSA 相关。尽管主要表现为低/中级癌症,但超过一半的 APCA 男性在手术中得到了升级,略多于 40% 的患者具有阳性切缘和/或前列腺外疾病。当与一组后部优势肿瘤相匹配时,前列腺切除术后生化失败率没有差异。
更新日期:2020-01-03
中文翻译:

前优势前列腺癌的临床病理特征和结果:对诊断和治疗的影响。
目的 本研究旨在描述在接受根治性前列腺切除术治疗局限性前列腺癌的男性中,与后/后外侧优势前列腺癌 (PPCA) 相比,前优势前列腺癌 (APCA) 的病理特征和临床结果。方法 这是一项单一机构、匹配的病例对照分析,对根据根治性前列腺切除术的病理肿瘤位置分层的短期临床结果进行分析。由专家泌尿生殖病理学家提取的关于肿瘤位置的病理数据与来自前瞻性机构数据库的临床和肿瘤结果数据相关联以进行分析。结果 从 2005 年到 2013 年,确定了 1580 名患者进行分析,其中 150 名 (9.5%) 患有 APCA。这些 APCA 男性中有 132 名拥有完整的临床数据,并与 353 名患有 PPCA 的男性相匹配(~1:3 比率)通过手术、切缘状态和病理 T 分期的 GrdGrp。APCA 和 PPCA 之间没有种族/民族差异(p = 0.13)。患有 APCA 的男性在诊断时表现出较高的 PSA 中值(6.4 [4.6-9.1] ng/mL vs 5.6 [4.4-8.1] ng/mL;p = 0.04),诊断时 GrdGrp 1 疾病发生率更高(57.7% vs. 40.0%,p = 0.003),与 PPCA 相比,直肠指检 (DRE) 异常率较低(10.1% 对 23.2%,p = 0.003)。与 PPCA 相比,APCA 男性的手术升级率更高(55.3% 对 42.0%,p = 0.015)。APCA 的 5 年无生化失败 (BF) 率为 85.1% (95% CI 73.1-98.9),患有 PPCA 的男性为 82.9% (95% CI 69.2-99.5)(p = 0.70,对数秩检验)。结论 大多数前部肿瘤无法通过 DRE 检测到,并且与诊断时较高的 PSA 相关。尽管主要表现为低/中级癌症,但超过一半的 APCA 男性在手术中得到了升级,略多于 40% 的患者具有阳性切缘和/或前列腺外疾病。当与一组后部优势肿瘤相匹配时,前列腺切除术后生化失败率没有差异。











































 京公网安备 11010802027423号
京公网安备 11010802027423号