当前位置:
X-MOL 学术
›
npj Prim. Care Respir. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Accuracy of Vitalograph lung monitor as a screening test for COPD in primary care.
npj Primary Care Respiratory Medicine ( IF 3.1 ) Pub Date : 2020-01-03 , DOI: 10.1038/s41533-019-0158-2 A P Dickens 1 , D A Fitzmaurice 2 , P Adab 1 , A Sitch 1 , R D Riley 3 , A Enocson 1 , R E Jordan 1
npj Primary Care Respiratory Medicine ( IF 3.1 ) Pub Date : 2020-01-03 , DOI: 10.1038/s41533-019-0158-2 A P Dickens 1 , D A Fitzmaurice 2 , P Adab 1 , A Sitch 1 , R D Riley 3 , A Enocson 1 , R E Jordan 1
Affiliation
|
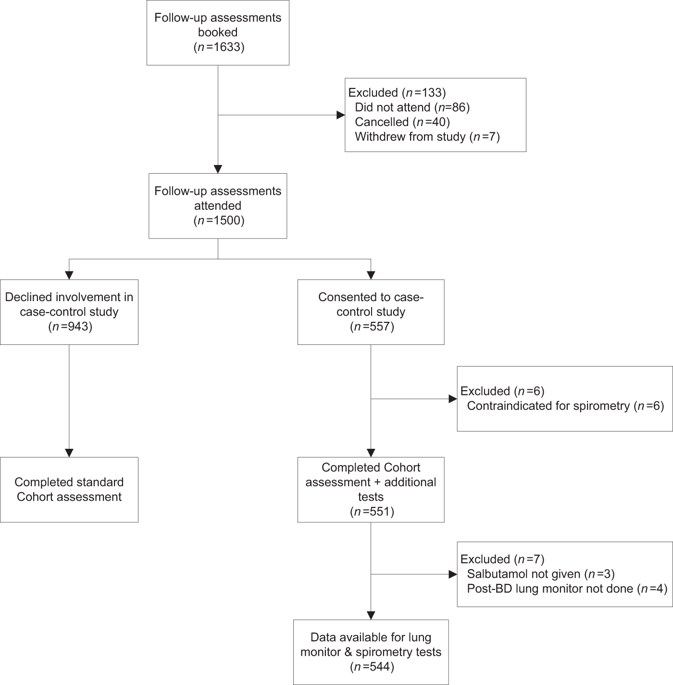
Microspirometry may be useful as the second stage of a screening pathway among patients reporting respiratory symptoms. We assessed sensitivity and specificity of the Vitalograph® lung monitor compared with post-bronchodilator confirmatory spirometry (ndd Easy on-PC) among primary care chronic obstructive pulmonary disease (COPD) patients within the Birmingham COPD cohort. We report a case-control analysis within 71 general practices in the UK. Eligible patients were aged ≥40 years who were either on a clinical COPD register or reported chronic respiratory symptoms on a questionnaire. Participants performed pre- and post-bronchodilator microspirometry, prior to confirmatory spirometry. Out of the 544 participants, COPD was confirmed in 337 according to post-bronchodilator confirmatory spirometry. Pre-bronchodilator, using the LLN as a cut-point, the lung monitor had a sensitivity of 50.5% (95% CI 45.0%, 55.9%) and a specificity of 99.0% (95% CI 96.6%, 99.9%) in our sample. Using a fixed ratio of FEV1/FEV6 < 0.7 to define obstruction in the lung monitor, sensitivity increased (58.8%; 95% CI 53.0, 63.8) while specificity was virtually identical (98.6%; 95% CI 95.8, 99.7). Within our sample, the optimal cut-point for the lung monitor was FEV1/FEV6 < 0.78, with sensitivity of 82.8% (95% CI 78.3%, 86.7%) and specificity of 85.0% (95% CI 79.4%, 89.6%). Test performance of the lung monitor was unaffected by bronchodilation. The lung monitor could be used in primary care without a bronchodilator using a simple ratio of FEV1/FEV6 as part of a screening pathway for COPD among patients reporting respiratory symptoms.
中文翻译:

Vitalograph 肺监测仪作为初级保健中 COPD 筛查测试的准确性。
显微肺活量测定法可能有助于作为报告呼吸道症状的患者筛查途径的第二阶段。我们在伯明翰 COPD 队列中的初级保健慢性阻塞性肺病 (COPD) 患者中评估了 Vitalograph® 肺监测仪与支气管扩张剂后确认性肺量计(ndd Easy on-PC)的敏感性和特异性。我们报告了英国 71 个全科诊所的病例对照分析。符合条件的患者年龄≥40岁,要么在临床慢性阻塞性肺病登记册上,要么在调查问卷上报告了慢性呼吸道症状。在确认性肺量测定之前,参与者进行了支气管扩张剂前后的微量肺量测定。在 544 名参与者中,根据支气管扩张剂后确认性肺量测定,337 名参与者被确诊患有慢性阻塞性肺病 (COPD)。使用支气管扩张剂前,使用 LLN 作为切点,在我们的研究中,肺监测仪的敏感性为 50.5%(95% CI 45.0%, 55.9%),特异性为 99.0%(95% CI 96.6%, 99.9%)。样本。使用固定比率 FEV1/FEV6 < 0.7 来定义肺部监测仪中的阻塞,敏感性增加 (58.8%; 95% CI 53.0, 63.8),而特异性几乎相同 (98.6%; 95% CI 95.8, 99.7)。在我们的样本中,肺部监测仪的最佳切点是 FEV1/FEV6 < 0.78,敏感性为 82.8% (95% CI 78.3%, 86.7%),特异性为 85.0% (95% CI 79.4%, 89.6%) )。肺部监测仪的测试性能不受支气管扩张的影响。肺部监测仪可用于初级保健,无需使用支气管扩张剂,使用 FEV1/FEV6 的简单比率作为报告呼吸道症状的患者中 COPD 筛查途径的一部分。
更新日期:2020-01-03
中文翻译:

Vitalograph 肺监测仪作为初级保健中 COPD 筛查测试的准确性。
显微肺活量测定法可能有助于作为报告呼吸道症状的患者筛查途径的第二阶段。我们在伯明翰 COPD 队列中的初级保健慢性阻塞性肺病 (COPD) 患者中评估了 Vitalograph® 肺监测仪与支气管扩张剂后确认性肺量计(ndd Easy on-PC)的敏感性和特异性。我们报告了英国 71 个全科诊所的病例对照分析。符合条件的患者年龄≥40岁,要么在临床慢性阻塞性肺病登记册上,要么在调查问卷上报告了慢性呼吸道症状。在确认性肺量测定之前,参与者进行了支气管扩张剂前后的微量肺量测定。在 544 名参与者中,根据支气管扩张剂后确认性肺量测定,337 名参与者被确诊患有慢性阻塞性肺病 (COPD)。使用支气管扩张剂前,使用 LLN 作为切点,在我们的研究中,肺监测仪的敏感性为 50.5%(95% CI 45.0%, 55.9%),特异性为 99.0%(95% CI 96.6%, 99.9%)。样本。使用固定比率 FEV1/FEV6 < 0.7 来定义肺部监测仪中的阻塞,敏感性增加 (58.8%; 95% CI 53.0, 63.8),而特异性几乎相同 (98.6%; 95% CI 95.8, 99.7)。在我们的样本中,肺部监测仪的最佳切点是 FEV1/FEV6 < 0.78,敏感性为 82.8% (95% CI 78.3%, 86.7%),特异性为 85.0% (95% CI 79.4%, 89.6%) )。肺部监测仪的测试性能不受支气管扩张的影响。肺部监测仪可用于初级保健,无需使用支气管扩张剂,使用 FEV1/FEV6 的简单比率作为报告呼吸道症状的患者中 COPD 筛查途径的一部分。











































 京公网安备 11010802027423号
京公网安备 11010802027423号