JAMA Surgery ( IF 15.7 ) Pub Date : 2019-02-01 , DOI: 10.1001/jamasurg.2018.3863 John C McAuliffe 1 , Laura H Tang 2 , Kambiz Kamrani 3 , Kelly Olino 4 , David S Klimstra 2 , Murray F Brennan 5 , Daniel G Coit 5
|
Importance Intraoperative consultation (IOC) on surgical margins during curative intent resection of gastric and gastroesophageal adenocarcinoma presents sampling and interpretive challenges. A false-negative (FN) IOC result can affect clinical care. Many factors may be associated with higher risk for an FN result of IOC on surgical margins.
Objective To assess the prevalence and clinical implications of FN results of IOC on surgical margins during resection of gastric and gastroesophageal adenocarcinoma.
Design, Setting, and Participants This retrospective study assessed the results of IOC on surgical margins to determine the prevalence of FN results and the accuracy and clinical implications of the results for patients undergoing curative intent resection for gastric or gastroesophageal adenocarcinoma. The study examined patients with gastric or gastroesophageal adenocarcinoma who underwent resection with curative intent at a single-institution referral center from January 1, 1992, to December 31, 2015.
Interventions Curative intent gastric and/or esophageal resection.
Main Outcomes and Measures False-negative results of IOC on surgical margins, accuracy of the results, factors associated with decreased accuracy of the results, and clinical implications of FN results.
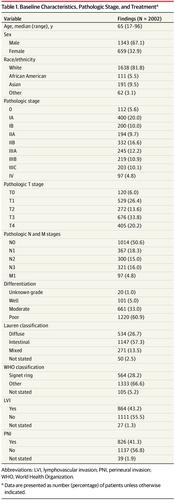
Results This study included 2002 patients (median age, 65 years; 1343 [67.1%] male; 1638 [81.8%] white) who received 3171 IOCs on surgical margins. Of the 3171 IOCs, the prevalence of FN results was 1.7%, with an accuracy of 98.1%. The prevalence of an FN IOC result was 1.2% for esophageal margins, 2.0% for gastric margins, and 2.5% for duodenal margins (P = .04). The prevalence of an FN IOC result was higher for patients with diffuse or signet ring disease compared with those without (2.6% vs 1.2%, P = .002) and for those not receiving neoadjuvant radiotherapy compared with those receiving neoadjuvant radiotherapy (1.4% vs 0.7%, P < .001). The prevalence of FN results of IOCs performed by nongastrointestinal pathologists was similar to that of IOCs performed by gastrointestinal pathologists (2.3% vs 1.9%, P = .60). The disease-specific survival was 34 months (95% CI, 20.7-47.2 months) for those with an FN result and 26.9 months (95% CI, 18.3-35.4; P = .72) for those with a true-positive result. Half of the patients with FN IOC results received further margin-directed therapy, including subsequent resection or radiotherapy.
Conclusions and Relevance This study found that IOC on surgical margins was accurate at a specialty center. Signet ring or diffuse disease, duodenal margins, and not receiving neoadjuvant radiotherapy were challenging scenarios for IOC on surgical margins. The use of IOC on surgical margins may be optimal when it will affect intraoperative decision making framed by the stage of disease, tumor location, and surgical fitness of the patient.
中文翻译:

胃及胃食管腺癌切除术中手术切缘术中咨询的假阴性结果普遍存在。
重要性 胃和胃食管腺癌的根治性切除术中手术切缘的术中咨询(IOC)带来了采样和解释方面的挑战。假阴性(FN)IOC结果可能会影响临床护理。许多因素可能与手术切缘上IOC的FN结果的较高风险有关。
目的 评估胃癌和胃食管腺癌切除过程中IOC FN结果对手术切缘的影响及其临床意义。
设计,设置和参加者 这项回顾性研究评估了IOC在手术切缘上的结果,以确定FN结果的普遍性以及该结果对胃或胃食管腺癌进行根治性切除的患者的准确性和临床意义。该研究对1992年1月1日至2015年12月在单机构转诊中心接受根治性切除术的胃或胃食管腺癌患者进行了检查。
干预 胃和/或食管切除术的意图性治疗。
主要结果和措施 IOC对手术切缘的假阴性结果,结果的准确性,与结果准确性降低相关的因素以及FN结果的临床意义。
结果 该研究纳入2002例患者(手术年龄中位数65岁;男性1343 [67.1%];白人1638 [81.8%]),接受了3171例IOC。在3171个IOC中,FN结果的患病率为1.7%,准确度为98.1%。FN IOC结果的发生率在食管切缘为1.2%,在胃切缘为2.0%,在十二指肠切缘为2.5%(P = 0.04)。弥漫性或印戒性疾病患者的FN IOC结果患病率高于无弥散性或印戒性疾病的患者(2.6%比1.2%,P = .002),未接受新辅助放疗的患者比接受新辅助放疗的患者(1.4%vs磷0.7% <.001)。非胃肠道病理学家进行的IOC的FN结果的发生率与胃肠道病理学家进行的IOC的发生率相似(2.3%对1.9%,P = 0.60)。FN结果患者的疾病特异性生存期为34个月(95%CI,20.7-47.2个月),而 真正阳性结果患者的疾病特异性生存期为26.9个月(95%CI,18.3-35.4;P = .72)。FN IOC结果的一半患者接受了进一步的切缘导向治疗,包括随后的切除或放疗。
结论与相关性 这项研究发现,在专科中心进行手术切缘的IOC是准确的。对于手术边缘的IOC,印戒或弥漫性疾病,十二指肠切缘以及未接受新辅助放疗是具有挑战性的方案。当在手术边缘使用IOC可能会影响疾病阶段,肿瘤位置和患者的手术适应度,从而影响术中决策时,可能是最佳的选择。











































 京公网安备 11010802027423号
京公网安备 11010802027423号