Theranostics ( IF 12.4 ) Pub Date : 2018-09-29 , DOI: 10.7150/thno.26193 Huan Wang , Yang Yang , Xin Sun , Fang Tian , Shuyuan Guo , Wei Wang , Zhen Tian , Hong Jin , Zhiguo Zhang , Ye Tian
|
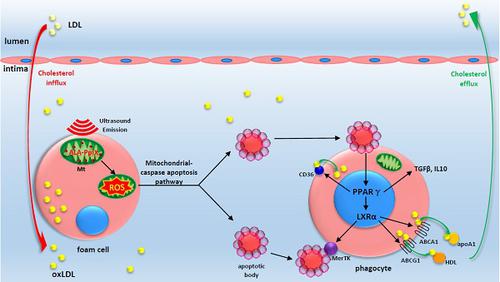
In advanced atherosclerotic plaques, defective efferocytosis of apoptotic foam cells and decreased cholesterol efflux contribute to lesion progression. In our previous study, we demonstrated that 5-aminolevulinic acid (ALA)-mediated sonodynamic therapy (SDT) could induce foam cells apoptosis via the mitochondrial-caspase pathway. In the current research, we sought to explore ALA-SDT-induced apoptosis of phagocytes and the effects of cholesterol efflux and efferocytosis in advanced apoE-/- mice plaque.
Methods: apoE-/- mice fed western diet were treated with ALA-SDT and sacrificed at day 1, day 3, day 7 and day 28 post treatment. THP-1 macrophage-derived foam cells were treated with ALA-SDT. 5 hours later, the supernatant was collected and added to fresh foam cells (phagocytes). Then, the lipid area, efferocytosis, cholesterol efflux, anti-inflammatory reactions and PPARγ-LXRα-ABCA1/ABCG1 pathway were detected in plaque in vivo and in phagocytes in vitro.
Results: We found that ALA-SDT induced foam cells apoptosis coupled with efferocytosis and upregulation of Mer tyrosine kinase (MerTK) both in vivo and in vitro. The lipid content in plaque decreased as early as 1 day after ALA-SDT and this tendency persisted until 28 days. The enhancement of phagocytes cholesterol efflux was accompanied by an approximately 40% decrease in free cholesterol and a 24% decrease in total cholesterol in vitro. More importantly, anti-inflammatory factors such as TGFβ and IL-10 were upregulated by ALA-SDT treatment. Finally, we found that PPARγ-LXRα-ABCA1/ABCG1 pathway was activated both in vivo and in vitro by ALA-SDT, which could be blocked by PPARγ siRNA.
Conclusions: Activation of PPARγ-LXRα-ABCA1/ABCG1 pathway induced by ALA-SDT treatment engages a virtuous cycle that enhances efferocytosis, cholesterol efflux and anti-inflammatory reactions in advanced plaque in vivo and in phagocytes in vitro.
Keywords: atherosclerosis, foam cells, sonodynamic therapy, phagocyte, cholesterol efflux
中文翻译:

声动力学疗法诱导的泡沫细胞凋亡激活吞噬性PPARγ-LXRα-ABCA1/ ABCG1途径并促进晚期斑块中的胆固醇外流
在晚期的动脉粥样硬化斑块中,凋亡性泡沫细胞的缺陷性红细胞增多症和胆固醇外排减少导致了病变的进展。在我们以前的研究中,我们证明了5-氨基乙酰丙酸(ALA)介导的声动力学疗法(SDT)可以通过线粒体半胱天冬酶途径诱导泡沫细胞凋亡。在当前的研究中,我们试图探索ALA-SDT诱导的吞噬细胞凋亡以及在晚期apoE -/-小鼠斑块中胆固醇外流和胞吞作用的影响。
方法:用ALA-SDT处理喂食西方饮食的apoE -/-小鼠,并在治疗后第1天,第3天,第7天和第28天处死。用ALA-SDT处理源自THP-1巨噬细胞的泡沫细胞。5小时后,收集上清液并加入新鲜的泡沫细胞(吞噬细胞)中。然后,在体内噬斑和体外吞噬细胞中检测脂质面积,血细胞增多,胆固醇流出,抗炎反应和PPARγ-LXRα-ABCA1/ ABCG1途径。
结果:我们发现,ALA-SDT在体内和体外均可诱导泡沫细胞凋亡,并伴有胞吞作用和Mer酪氨酸激酶(MerTK)的上调。斑块中的脂质含量最早在ALA-SDT后1天下降,这种趋势一直持续到28天。吞噬细胞胆固醇外排的增强伴随着游离胆固醇的降低约40%,体外总胆固醇的降低约24%。更重要的是,ALA-SDT处理可上调抗炎因子,例如TGFβ和IL-10。最后,我们发现ALA-SDT在体内和体外均激活了PPARγ-LXRα-ABCA1/ ABCG1途径,该途径可能被PPARγsiRNA阻断。
结论: ALA-SDT处理诱导的PPARγ-LXRα-ABCA1/ ABCG1途径的激活参与了一个良性循环,增强了体内和体外吞噬晚期斑块的胞吐作用,胆固醇外排和抗炎反应。
关键词:动脉粥样硬化,泡沫细胞,声动力学治疗,吞噬细胞,胆固醇外流











































 京公网安备 11010802027423号
京公网安备 11010802027423号