当前位置:
X-MOL 学术
›
JAMA Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Effect of Depth of Sedation in Older Patients Undergoing Hip Fracture Repair on Postoperative Delirium: The STRIDE Randomized Clinical Trial.
JAMA Surgery ( IF 15.7 ) Pub Date : 2018-11-01 , DOI: 10.1001/jamasurg.2018.2602 Frederick E Sieber 1 , Karin J Neufeld 2 , Allan Gottschalk 3, 4 , George E Bigelow 5 , Esther S Oh 6 , Paul B Rosenberg 2 , Simon C Mears 7 , Kerry J Stewart 8 , Jean-Pierre P Ouanes 3 , Mahmood Jaberi 1 , Erik A Hasenboehler 9 , Tianjing Li 10 , Nae-Yuh Wang 11
JAMA Surgery ( IF 15.7 ) Pub Date : 2018-11-01 , DOI: 10.1001/jamasurg.2018.2602 Frederick E Sieber 1 , Karin J Neufeld 2 , Allan Gottschalk 3, 4 , George E Bigelow 5 , Esther S Oh 6 , Paul B Rosenberg 2 , Simon C Mears 7 , Kerry J Stewart 8 , Jean-Pierre P Ouanes 3 , Mahmood Jaberi 1 , Erik A Hasenboehler 9 , Tianjing Li 10 , Nae-Yuh Wang 11
Affiliation
|
Importance
Postoperative delirium is the most common complication following major surgery in older patients. Intraoperative sedation levels are a possible modifiable risk factor for postoperative delirium.
Objective
To determine whether limiting sedation levels during spinal anesthesia reduces incident delirium overall.
Design, Setting, and Participants
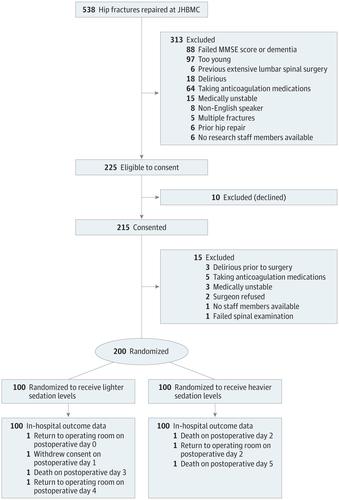
This double-blind randomized clinical trial (A Strategy to Reduce the Incidence of Postoperative Delirum in Elderly Patients [STRIDE]) was conducted from November 18, 2011, to May 19, 2016, at a single academic medical center and included a consecutive sample of older patients (≥65 years) who were undergoing nonelective hip fracture repair with spinal anesthesia and propofol sedation. Patients were excluded for preoperative delirium or severe dementia. Of 538 hip fractures screened, 225 patients (41.8%) were eligible, 10 (1.9%) declined participation, 15 (2.8%) became ineligible between the time of consent and surgery, and 200 (37.2%) were randomized. The follow-up included postoperative days 1 to 5 or until hospital discharge.
Interventions
Heavier (modified observer's assessment of sedation score of 0-2) or lighter (observer's assessment of sedation score of 3-5) propofol sedation levels intraoperatively.
Main Outcomes and Measures
Delirium on postoperative days 1 to 5 or until hospital discharge determined via consensus panel using Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) criteria. The incidence of delirium was compared between intervention groups with and without stratification by the Charlson comorbidity index (CCI).
Results
Of 200 participants, the mean (SD) age was 82 (8) years, 146 (73%) were women, 194 (97%) were white, and the mean (SD) CCI was 1.5 (1.8). One hundred participants each were randomized to receive lighter sedation levels or heavier sedation levels. A good separation of intraoperative sedation levels was confirmed by multiple indices. The overall incident delirium risk was 36.5% (n = 73) and 39% (n = 39) vs 34% (n = 34) in heavier and lighter sedation groups, respectively (P = .46). Intention-to-treat analyses indicated no statistically significant difference between groups in the risk of incident delirium (log-rank test χ2, 0.46; P = .46). However, in a prespecified subgroup analysis, when stratified by CCI, sedation levels did effect the delirium risk (P for interaction = .04); in low comorbid states (CCI = 0), heavier vs lighter sedation levels doubled the risk of delirium (hazard ratio, 2.3; 95% CI, 1.1- 4.9). The level of sedation did not affect delirium risk with a CCI of more than 0.
Conclusions and Relevance
In the primary analysis, limiting the level of sedation provided no significant benefit in reducing incident delirium. However, in a prespecified subgroup analysis, lighter sedation levels benefitted reducing postoperative delirium for persons with a CCI of 0.
Trial Registration
clinicaltrials.gov Identifier: NCT00590707.
中文翻译:

髋部骨折修复术对老年患者镇静深度的影响对术后Deli妄的影响:STRIDE随机临床试验。
重要性术后del妄是老年患者大手术后最常见的并发症。术中镇静水平可能是术后del妄的可能危险因素。目的确定在麻醉过程中限制镇静水平是否能降低整体incident妄。设计,背景和参与者这项双盲随机临床试验(一项降低老年患者术后弹药发生率的策略[STRIDE])于2011年11月18日至2016年5月19日,在一个学术医学中心进行。并包括连续样本的老年患者(≥65岁),他们接受了脊髓麻醉和异丙酚镇静术进行的非选择性髋部骨折修复。患者因术前ir妄或严重痴呆而被排除在外。在538例筛查的髋部骨折中,225例患者(41.8%)符合条件,10例(1.9%)拒绝参与,15例(2.8%)在同意和手术之间不符合条件,200例(37.2%)被随机分配。随访包括术后1至5天或直至出院。干预术中丙泊酚镇静水平较重(观察者的镇静分数评估为0-2改良)或较轻(观察者的镇静分数为3-5评估)。主要结果和措施术后1至5天或直至出院后,由共识小组使用《精神疾病诊断和统计手册》(第四版,文本修订)标准确定Deli妄。通过查尔森合并症指数(CCI)比较了有分层和无分层干预组之间的ir妄发生率。200名参与者的结果,平均(SD)年龄为82(8)岁,女性为146(73%),白人为194(97%),平均CCI为1.5(1.8)。将一百名参与者随机分为两组,分别接受较轻的镇静水平或较重的镇静水平。多个指标证实了术中镇静水平的良好分离。较重镇静组和较轻镇静组的总incident妄发生风险分别为36.5%(n = 73)和39%(n = 39),而在较轻和较轻的镇静组中分别为34%(n = 34)(P = 0.46)。意向性治疗分析表明,两组之间发生ir妄的风险无统计学差异(对数秩检验χ2,0.46; P = 0.46)。但是,在预先指定的亚组分析中,当按CCI进行分层时,镇静水平确实会影响ir妄风险(相互作用的P = .04)。在低合并症状态下(CCI = 0),较重与较轻的镇静水平使of妄的风险增加一倍(危险比,2.3; 95%CI,1.1-4.9)。镇静水平不影响CCI大于0的del妄风险。结论和相关性在最初的分析中,限制镇静水平对减少incident妄没有明显的益处。但是,在预先指定的亚组分析中,较轻的镇静水平有益于CCI为0的患者减少术后del妄。试验注册临床试验.gov标识符:NCT00590707。
更新日期:2018-11-24
中文翻译:

髋部骨折修复术对老年患者镇静深度的影响对术后Deli妄的影响:STRIDE随机临床试验。
重要性术后del妄是老年患者大手术后最常见的并发症。术中镇静水平可能是术后del妄的可能危险因素。目的确定在麻醉过程中限制镇静水平是否能降低整体incident妄。设计,背景和参与者这项双盲随机临床试验(一项降低老年患者术后弹药发生率的策略[STRIDE])于2011年11月18日至2016年5月19日,在一个学术医学中心进行。并包括连续样本的老年患者(≥65岁),他们接受了脊髓麻醉和异丙酚镇静术进行的非选择性髋部骨折修复。患者因术前ir妄或严重痴呆而被排除在外。在538例筛查的髋部骨折中,225例患者(41.8%)符合条件,10例(1.9%)拒绝参与,15例(2.8%)在同意和手术之间不符合条件,200例(37.2%)被随机分配。随访包括术后1至5天或直至出院。干预术中丙泊酚镇静水平较重(观察者的镇静分数评估为0-2改良)或较轻(观察者的镇静分数为3-5评估)。主要结果和措施术后1至5天或直至出院后,由共识小组使用《精神疾病诊断和统计手册》(第四版,文本修订)标准确定Deli妄。通过查尔森合并症指数(CCI)比较了有分层和无分层干预组之间的ir妄发生率。200名参与者的结果,平均(SD)年龄为82(8)岁,女性为146(73%),白人为194(97%),平均CCI为1.5(1.8)。将一百名参与者随机分为两组,分别接受较轻的镇静水平或较重的镇静水平。多个指标证实了术中镇静水平的良好分离。较重镇静组和较轻镇静组的总incident妄发生风险分别为36.5%(n = 73)和39%(n = 39),而在较轻和较轻的镇静组中分别为34%(n = 34)(P = 0.46)。意向性治疗分析表明,两组之间发生ir妄的风险无统计学差异(对数秩检验χ2,0.46; P = 0.46)。但是,在预先指定的亚组分析中,当按CCI进行分层时,镇静水平确实会影响ir妄风险(相互作用的P = .04)。在低合并症状态下(CCI = 0),较重与较轻的镇静水平使of妄的风险增加一倍(危险比,2.3; 95%CI,1.1-4.9)。镇静水平不影响CCI大于0的del妄风险。结论和相关性在最初的分析中,限制镇静水平对减少incident妄没有明显的益处。但是,在预先指定的亚组分析中,较轻的镇静水平有益于CCI为0的患者减少术后del妄。试验注册临床试验.gov标识符:NCT00590707。










































 京公网安备 11010802027423号
京公网安备 11010802027423号