JAMA Surgery ( IF 15.7 ) Pub Date : 2018-10-01 , DOI: 10.1001/jamasurg.2018.1680 Stephen B. Williams 1 , Yong Shan 1 , Usama Jazzar 1 , Hemalkumar B. Mehta 2 , Jacques G. Baillargeon 3 , Jinhai Huo 4 , Anthony J. Senagore 2 , Eduardo Orihuela 1 , Douglas S. Tyler 2 , Todd A. Swanson 5 , Ashish M. Kamat 6
|
Importance Radical cystectomy is the guidelines-recommended treatment of muscle-invasive bladder cancer, but a resurgence of trimodal therapy has occurred. Limited comparative data are available on outcomes and costs attributable to these 2 treatments.
Objective To compare the survival outcomes and costs between trimodal therapy and radical cystectomy in older adults with muscle-invasive bladder cancer.
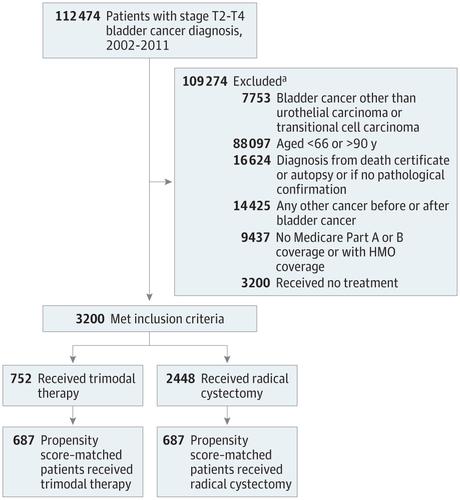
Design, Setting, and Participants This population-based cohort study used data from the Surveillance, Epidemiology, and End Results–Medicare linked database. A total of 3200 older adults (aged ≥66 years) with clinical stage T2 to T4a bladder cancer diagnosed from January 1, 2002, to December 31, 2011, and with claims data available through December 31, 2013, were included in the analysis. Patients who received radical cystectomy underwent either only surgery or surgery in combination with radiotherapy or chemotherapy. Patients who received trimodal therapy underwent transurethral resection of the bladder followed by radiotherapy and chemotherapy. Propensity score matching by sociodemographic and clinical characteristics was used. Data analysis was performed from August 1, 2017, to March 11, 2018.
Main Outcomes and Measures Overall survival and cancer-specific survival were evaluated using the Cox proportional hazards regression model and the Fine and Gray competing risk model. All Medicare health care costs for inpatient, outpatient, and physician services within 30, 90, and 180 days of treatment were compared. The total amount spent nationwide was estimated, using 180-day medical costs between treatments, by the total number of new cases of muscle-invasive bladder cancer in the United States in 2011.
Results Of the 3200 patients who met the inclusion criteria, 2048 (64.0%) were men and 1152 (36.0%) were women, with a mean (SD) age of 75.8 (6.0) years. After propensity score matching, 687 patients (21.5%) underwent trimodal therapy and 687 patients (21.5%) underwent radical cystectomy. Patients who underwent trimodal therapy had significantly decreased overall survival (hazard ratio [HR], 1.49; 95% CI, 1.31-1.69) and cancer-specific survival (HR, 1.55; 95% CI, 1.32-1.83). No differences in costs at 30 days were observed between trimodal therapy ($15 233 in 2002 vs $18 743 in 2011) and radical cystectomy ($17 990 in 2002 vs $21 738 in 2011). However, median total costs were significantly higher with trimodal therapy than with radical cystectomy at 90 days ($80 174 vs $69 181; median difference, $8964; Hodges-Lehmann 95% CI, $3848-$14 079) and at 180 days ($179 891 vs $107 017; median difference, $63 771; Hodges-Lehmann 95% CI, $55 512-$72 029). Extrapolating these figures to the total US population revealed $335 million in excess spending for trimodal therapy compared with the less costly radical cystectomy ($492 million) for patients who received a muscle-invasive bladder cancer diagnosis in 2011.
Conclusions and Relevance Trimodal therapy was associated with significantly decreased overall survival and cancer-specific survival as well as $335 million in excess spending in 2011. These findings have important health policy implications regarding the appropriate use of high value–based care among older adults with invasive bladder cancer who are candidates for either radical cystectomy or trimodal therapy.
中文翻译:

膀胱浸润性膀胱癌的成年人的根治性膀胱切除术和三峰疗法相关的生存结果和费用的比较
重要性 根治性膀胱切除术是指南推荐的肌肉浸润性膀胱癌的治疗方法,但三峰疗法已复活。关于这两种治疗的结果和费用,可获得的比较数据有限。
目的 比较三联疗法和根治性膀胱切除术对老年肌浸润性膀胱癌患者的生存结局和费用。
设计,环境和参与者 这项基于人群的队列研究使用了来自“监测”,“流行病学”和“最终结果-医疗保险”链接数据库的数据。分析包括2002年1月1日至2011年12月31日诊断为临床T2至T4a膀胱癌的3200名老年人(年龄≥66岁),并提供截至2013年12月31日的索赔数据。接受根治性膀胱切除术的患者仅接受手术或联合放疗或化疗的手术。接受三联疗法的患者先行膀胱尿道切除术,然后进行放射疗法和化学疗法。使用通过社会人口统计学和临床特征进行的倾向得分匹配。数据分析于2017年8月1日至2018年3月11日进行。
主要结果和措施 使用Cox比例风险回归模型以及Fine和Gray竞争风险模型评估总体生存期和癌症特异性生存期。比较了在治疗30、90和180天内住院,门诊和医师服务的所有Medicare医疗保健费用。根据2011年美国新发肌肉浸润性膀胱癌病例数,使用两次治疗之间的180天医疗费用,估算了全国的总支出。
结果 符合入选标准的3200名患者中,男性2048名(64.0%),女性1152名(36.0%),平均(SD)年龄为75.8(6.0)岁。倾向评分匹配后,有687例患者(21.5%)接受了三峰疗法,而有687例患者(21.5%)接受了根治性膀胱切除术。接受三联疗法的患者的总生存期(危险比[HR]为1.49; 95%CI为1.31-1.69)和癌症特异性生存期(HR为1.55; 95%CI为1.32-1.83)显着降低。三联疗法(2002年为15 233美元,2011年为18 743美元)和根治性膀胱切除术(2002年为17 990美元,2011年为21 738美元)在30天时没有观察到费用差异。然而,在90天时,三模式疗法的总费用中位数比根治性膀胱切除术要高得多(80 174美元vs 69 181美元;中位数差异为8964美元; Hodges-Lehmann 95%CI,$ 3848- $ 14 079)和180天($ 179 891比$ 107 017;中位数差,$ 63 771; Hodges-Lehmann 95%CI,$ 55 512- $ 72 029)。将这些数字推算到美国总人口中,与2011年接受肌肉浸润性膀胱癌诊断的患者进行的根治性膀胱切除术(费用较低)(4.92亿美元)相比,三峰疗法的额外支出为3.35亿美元。
结论与相关性 2011年,三态疗法与整体生存率和癌症特异性生存率显着降低以及3.35亿美元的超支支出相关。这些发现对健康的政策具有重要的意义,涉及在患有侵入性疾病的老年人中适当使用基于高价值的护理膀胱癌,可以进行根治性膀胱切除术或三联疗法。











































 京公网安备 11010802027423号
京公网安备 11010802027423号