JAMA Surgery ( IF 15.7 ) Pub Date : 2018-08-01 , DOI: 10.1001/jamasurg.2018.1039 Shahid Shafi 1 , Ashley W. Collinsworth 1, 2 , Laurel A. Copeland 3 , Gerald O. Ogola 1 , Taoran Qiu 1 , Maria Kouznetsova 1 , I-Chia Liao 3 , Natalie Mears 3 , An T. Pham 4, 5 , George J. Wan 4 , Andrew L. Masica 1
|
Importance Opioids are commonly used for pain control during and after invasive procedures. However, opioid-related adverse drug events (ORADEs) are common and have been associated with worse patient outcomes.
Objectives To examine the incidence of ORADEs in patients undergoing hospital-based surgical and endoscopic procedures and to evaluate the association of ORADEs with clinical and cost outcomes.
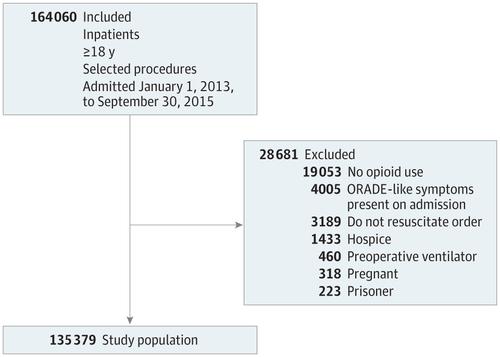
Design, Setting, and Participants In this retrospective study of clinical and administrative data, ORADEs were identified using International Classification of Diseases, Ninth Revision diagnosis codes for known adverse effects of opioids or by opioid antagonist use. Multivariable regression analysis was used to measure the association of ORADEs with outcomes after adjusting for potential confounding factors. The setting was 21 acute care hospitals in a large integrated health care delivery system. Participants were 135 379 patients (aged ≥18 years, admitted from January 1, 2013, to September 30, 2015) who underwent surgical and endoscopic procedures and were given opioids.
Exposure Opioid use, reported as morphine milligram equivalent doses.
Main Outcomes and Measures Opioid-related adverse drug events and their association with inpatient mortality, discharge to another care facility, length of stay, cost of hospitalization, and 30-day readmission.
Results Among 135 379 adult patients in this study (67.5% female), 14 386 (10.6%) experienced at least one ORADE. Patients with ORADEs were more likely to be older, of white race/ethnicity, and male and have more comorbidities. Patients with ORADEs received a higher total dose of opioids (median morphine milligram equivalent dose, 46.8 vs 30.0 mg; P < .001) and for a longer duration (median, 3.0 vs 2.0 days; P < .001). In adjusted analyses, ORADEs were associated with increased inpatient mortality (odds ratio [OR], 28.8; 95% CI, 24.0-34.5), greater likelihood of discharge to another care facility (OR, 2.9; 95% CI, 2.7-3.0), prolonged length of stay (OR, 3.1; 95% CI, 2.8-3.4), high cost of hospitalization (OR, 2.7; 95% CI, 2.4-3.0), and higher rate of 30-day readmission (OR, 1.3; 95% CI, 1.2-1.4). ORADEs were associated with a 2.9% increase in absolute mortality, an $8225 increase in cost for the index hospitalization, and a 1.6-day increase in length of stay for the index hospitalization.
Conclusions and Relevance Opioid-related adverse drug events were common among patients undergoing hospital-based invasive procedures and were associated with significantly worse clinical and cost outcomes. Hospital-acquired harm from ORADEs in the surgical patient population is an important opportunity for health systems to improve patient safety and reduce cost.
中文翻译:

阿片类药物相关不良药物事件与大型综合医疗服务系统中手术患者的临床和成本结果的关联
重要性 阿片类药物通常用于侵入性手术期间和之后的疼痛控制。但是,阿片类药物相关的不良药物事件(ORADE)很常见,并且与患者预后差有关。
目的 探讨接受基于外科手术和内窥镜手术的患者中ORADE的发生率,并评估ORADE与临床和成本结果之间的关系。
设计,背景和参与者 在这项临床和行政数据回顾性研究中,使用国际疾病分类,第九版诊断代码对阿片类药物的已知不良反应或使用阿片类药物拮抗剂进行了ORADE的鉴定。在对潜在的混杂因素进行调整之后,使用多变量回归分析来衡量ORADE与结果的关联。设置是在大型综合医疗保健提供系统中的21家急诊医院。参加手术和内窥镜检查并接受阿片类药物治疗的135379例患者(年龄≥18岁,自2013年1月1日至2015年9月30日入院)。
接触 阿片类药物的使用,以吗啡毫克当量剂量报道。
主要结果和措施 与阿片类药物有关的不良药物事件及其与住院死亡率,到另一家护理机构出院,住院时间,住院费用和30天再入院的关系。
结果 在该研究的135379名成年患者中(女性占67.5%),有14386名(10.6%)经历了至少一次ORADE。患有ORADE的患者更可能是年龄较大,具有白色种族/民族的患者以及男性,并且合并症更多。患有ORADE的患者接受更高剂量的阿片类药物(中度吗啡毫克当量剂量,分别为46.8和30.0 mg;P <.001)和更长的持续时间(中位,分别为3.0天和2.0天;P <.001)。在调整后的分析中,ORADE与住院死亡率增加相关(赔率[OR],28.8; 95%CI,24.0-34.5),出院到另一家医疗机构的可能性更大(OR,2.9; 95%CI,2.7-3.0) ,住院时间延长(OR,3.1; 95%CI,2.8-3.4),住院费用高(OR,2.7; 95%CI,2.4-3.0)和30天再入院率更高(OR,1.3; 95%CI,1.2-1.4)。ORADE与绝对死亡率增加2.9%,索引住院的费用增加$ 8225和索引住院的住院时间增加1.6天有关。
结论与相关性 阿片类药物相关的不良药物事件在以医院为基础的侵入性手术患者中很常见,并且与临床和成本结果显着恶化有关。ORADE对医院外科手术患者造成的伤害是医疗系统提高患者安全性和降低成本的重要机会。











































 京公网安备 11010802027423号
京公网安备 11010802027423号