JAMA Surgery ( IF 15.7 ) Pub Date : 2018-05-01 , DOI: 10.1001/jamasurg.2017.5928 Christopher S. Digesu 1 , Kathleen D. Weiss 1 , Yolonda L. Colson 1
|
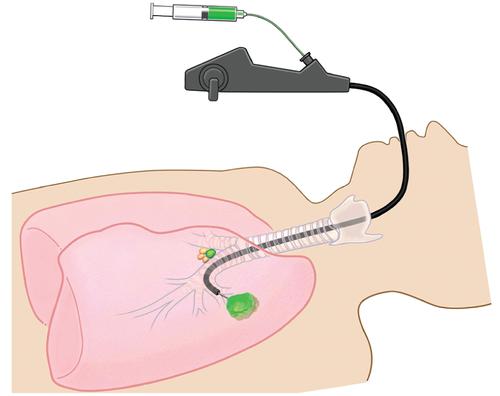
Non–small cell lung cancer (NSCLC) prognosis is linked to lymphatic spread of disease, but localizing metastatic disease within locoregional lymphatics to accurately stage and guide therapy represents a clinical challenge. This challenge is evident in the nearly 30% recurrence rate and suboptimal overall survival among patients thought to have early-stage disease.1 Complex thoracic lymphatic pathways and variable surgeon practices result in inadequate nodal analysis in nearly 50% of patients with lung cancer undergoing surgery.2 Furthermore, the current practice of hematoxylin and eosin staining of sampled nodes misses metastatic disease in up to 22% of patients.3 Sentinel lymph node (SLN) mapping allows surgeons to target the first tumor-draining lymph node for sampling and for in-depth pathologic analysis. Previous applications of SLN mapping in NSCLC have been met with variable success. However, recent advances in image-guided surgery, specifically near-infrared (NIR) imaging, have led to renewed interest in the diagnostic and therapeutic benefits of SLN mapping. Two phase 1, single-institution clinical trials examined real-time NIR SLN mapping after peritumoral injection of the NIR fluorescent dye indocyanine green in patients with NSCLC. These trials resulted in a greater than 80% detection of NIR-positive SLN(s) without adverse events and identified metastatic disease exclusively within the SLN in several patients.4,5 The fluorescence itself is physiologically independent of disease status and is intended to function as an anatomical indicator of the most clinically relevant node (ie, the first tumor-draining lymph node). To reach tumors of varying sizes and locations, several approaches have been developed for peritumoral indocyanine green injection, including transthoracic injection for palpable tumors and navigational bronchoscopy–guided (Figure) or intraoperative computed tomography–guided injections for small, ill-defined early-stage tumors.
中文翻译:

非小细胞肺癌的近红外前哨淋巴结鉴定
非小细胞肺癌(NSCLC)的预后与疾病的淋巴扩散有关,但是将转移性疾病局限在局部淋巴管内以准确地分期和指导治疗是一项临床挑战。在被认为患有早期疾病的患者中,近30%的复发率和次优总体生存率证明了这一挑战。1复杂的胸腔淋巴途径和外科医生的做法不一,导致近50%接受手术的肺癌患者的淋巴结分析不足。2此外,目前对苏木精和曙红染色的淋巴结的现行做法在多达22%的患者中错过了转移性疾病。3前哨淋巴结(SLN)映射使外科医生可以将第一个引流肿瘤的淋巴结作为目标,以便进行采样和进行深入的病理分析。SLN映射在NSCLC中的先前应用已获得了不同程度的成功。但是,图像引导手术,特别是近红外(NIR)成像的最新进展,引起了人们对SLN绘图的诊断和治疗益处的新兴趣。两项1期,单机构的临床试验研究了NSCLC患者肿瘤周围注射NIR荧光染料吲哚菁绿后的实时NIR SLN定位。这些试验导致对NIR阳性SLN的检出率超过80%,且无不良事件,并且仅在几名患者中在SLN内发现了转移性疾病。4 ,5荧光本身在生理上与疾病状态无关,并且旨在充当临床上最相关的淋巴结(即第一个引流肿瘤的淋巴结)的解剖指标。为了达到不同大小和位置的肿瘤,已针对肿瘤周围吲哚菁绿注射剂开发了几种方法,包括经胸腔注射可触及的肿瘤和导航支气管镜引导下(图)或术中计算机断层扫描引导下的小而不确定的早期注射肿瘤。











































 京公网安备 11010802027423号
京公网安备 11010802027423号