PLOS ONE ( IF 2.9 ) Pub Date : 2018-03-19 , DOI: 10.1371/journal.pone.0194675 Setegn Eshetie 1 , Mucheye Gizachew 1 , Animut Alebel 2 , Dick van Soolingen 3
|
Background
Knowledge of tuberculosis (TB) treatment outcomes is substantially needed to assess the performance of national TB controls programs (NTPs). To date, the overall estimates of treatment outcomes have not been determined in Ethiopia. Therefore, this meta-analysis was undertaken to produce pooled estimates of TB treatment outcomes and to analyze the impact of prior anti-TB drug exposure and HIV co-infection.
Methods
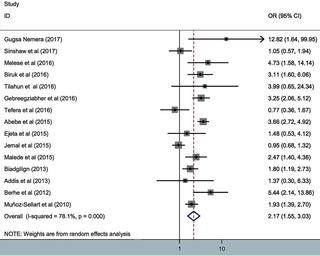
Potentially relevant studies were retrieved from PubMed, EMBASE, and MEDLINE online databases. The unpublished studies have been retrieved from the grey literature through Google and Google Scholar. The pooled estimates were calculated using random effect model. The summary estimates were also presented using Forest plots and Tables. The outcome measures were successful and unsuccessful treatment outcomes. Patients who were cured or with completed treatment defined as successful treatment outcome and patients meeting the definition of death, defaulting and failure are considered as unsuccessfully treated cases.
Results
A total of 34 studies are included for meta-analysis. The pooled estimate of successful TB treatment outcomes amounts to 83.7% (95% CI 81.1%–86.3%). Of successfully treated cases, 33.9% were cured and the remaining completed cases. Besides, among patients with unsuccessful treatment outcome, nearly 50% were dead and the rest were treatment failures and defaulters. Sub-group analysis shows that high treatment success rate was estimated in Afar; 88.9% (95% CI 83.8%–94.2%), followed by Oromia; 88.5% (95% CI 82.6%–94.5%) and Gambella; 86.1% (95% CI 84.4%–87.9%), whereas relatively poor treatment outcome was noted in Tigray; 20.0% (95% CI 2.1%–37.9%) and Amhara; 19.0% (95% CI 12.6%–25.5%). The unsuccessful TB treatment outcome was found to be higher among HIV/TB co-infected cases with an odds ratio of 1.98 (95%CI, 1.56–2.52) and re-treated cases with an odds ratio of 2.17 (95%CI, 1.55–3.03). The time trend was assessed from 2003 to 2016, but it shows insignificant variation with treatment outcome (P = 0.108).
Conclusion
The rate of successful treatment outcome in Ethiopia appears generally high, only slightly below the threshold suggested by the World Health Organization. History of tuberculosis treatment and HIV/TB co-infection were inversely associated with favorable treatment outcomes.
中文翻译:

2003年至2016年埃塞俄比亚的结核病治疗结果以及艾滋病毒合并感染和既往药物暴露的影响:系统评价和荟萃分析
背景
评估国家结核病控制规划(NTP)的绩效非常需要了解结核病(TB)治疗结果。迄今为止,埃塞俄比亚治疗结果的总体估计尚未确定。因此,进行这项荟萃分析是为了对结核病治疗结果进行汇总估计,并分析既往抗结核药物暴露和艾滋病毒合并感染的影响。
方法
从 PubMed、EMBASE 和 MEDLINE 在线数据库检索可能相关的研究。未发表的研究是通过谷歌和谷歌学术从灰色文献中检索出来的。使用随机效应模型计算汇总估计值。还使用森林图和表格呈现了汇总估计。结果指标包括成功和不成功的治疗结果。治愈或完成治疗定义为成功治疗结果的患者以及满足死亡、违约和失败定义的患者被视为治疗失败病例。
结果
总共纳入 34 项研究进行荟萃分析。结核病治疗成功率的汇总估计值为 83.7%(95% CI 81.1%–86.3%)。在成功治疗的病例中,治愈率为33.9%,其余病例已完成。此外,治疗失败的患者中,近50%死亡,其余为治疗失败和违约者。亚组分析显示,阿法尔的治疗成功率估计很高; 88.9%(95% CI 83.8%–94.2%),其次是奥罗米亚州; 88.5%(95% CI 82.6%–94.5%)和甘贝拉; 86.1% (95% CI 84.4%–87.9%),而提格雷的治疗结果相对较差; 20.0%(95% CI 2.1%–37.9%)和阿姆哈拉; 19.0%(95% CI 12.6%–25.5%)。研究发现,HIV/结核病合并感染病例的结核病治疗失败率较高,比值比为 1.98(95%CI,1.56–2.52),而再治疗病例的比值比为 2.17(95%CI,1.55)。 –3.03)。评估了 2003 年至 2016 年的时间趋势,但其随治疗结果变化不显着(P = 0.108)。
结论
埃塞俄比亚的治疗成功率普遍较高,仅略低于世界卫生组织建议的阈值。结核病治疗史和艾滋病毒/结核病合并感染与良好的治疗结果呈负相关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号