PLOS Neglected Tropical Diseases ( IF 3.4 ) Pub Date : 2018-03-12 , DOI: 10.1371/journal.pntd.0006281 Lloyd Einsiedel , Hai Pham , Kim Wilson , Rebecca Walley , Jocelyn Turpin , Charles Bangham , Antoine Gessain , Richard J. Woodman
|
Background
The Human T-Lymphotropic Virus type 1c subtype (HTLV-1c) is highly endemic to central Australia where the most frequent complication of HTLV-1 infection in Indigenous Australians is bronchiectasis. We carried out a prospective study to quantify the prognosis of HTLV-1c infection and chronic lung disease and the risk of death according to the HTLV-1c proviral load (pVL).
Methodology/Principal findings
840 Indigenous adults (discharge diagnosis of bronchiectasis, 154) were recruited to a hospital-based prospective cohort. Baseline HTLV-1c pVL were determined and the results of chest computed tomography and clinical details reviewed. The odds of an association between HTLV-1 infection and bronchiectasis or bronchitis/bronchiolitis were calculated, and the impact of HTLV-1c pVL on the risk of death was measured.
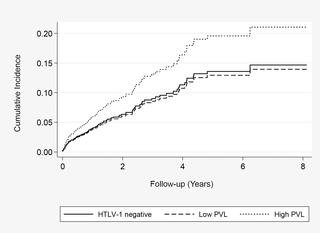
Radiologically defined bronchiectasis and bronchitis/bronchiolitis were significantly more common among HTLV-1-infected subjects (adjusted odds ratio = 2.9; 95% CI, 2.0, 4.3). Median HTLV-1c pVL for subjects with airways inflammation was 16-fold higher than that of asymptomatic subjects. There were 151 deaths during 2,140 person-years of follow-up (maximum follow-up 8.13 years). Mortality rates were higher among subjects with HTLV-1c pVL ≥1000 copies per 105 peripheral blood leukocytes (log-rank χ2 (2df) = 6.63, p = 0.036) compared to those with lower HTLV-1c pVL or uninfected subjects. Excess mortality was largely due to bronchiectasis-related deaths (adjusted HR 4.31; 95% CI, 1.78, 10.42 versus uninfected).
Conclusion/Significance
Higher HTLV-1c pVL was strongly associated with radiologically defined airways inflammation and with death due to complications of bronchiectasis. An increased risk of death due to an HTLV-1 associated inflammatory disease has not been demonstrated previously. Our findings indicate that mortality associated with HTLV-1c infection may be higher than has been previously appreciated. Further prospective studies are needed to determine whether these results can be generalized to other HTLV-1 endemic areas.
中文翻译:

澳大利亚原住民人群的人类T淋病病毒1c亚型前病毒载量,慢性肺疾病和生存率
背景
人类T型淋巴病毒1c型亚型(HTLV-1c)在澳大利亚中部高度流行,在澳大利亚中部,HTLV-1感染最常见的并发症是支气管扩张。我们进行了一项前瞻性研究,以根据HTLV-1c的前病毒载量(pVL)量化HTLV-1c感染和慢性肺病的预后以及死亡风险。
方法/主要发现
840名土著成年人(支气管扩张的出院诊断,154名)被招募到以医院为基础的前瞻性队列中。确定基线HTLV-1c pVL,并对胸部计算机断层扫描的结果和临床细节进行回顾。计算HTLV-1感染与支气管扩张或支气管炎/细支气管炎之间关联的几率,并测量HTLV-1c pVL对死亡风险的影响。
在受HTLV-1感染的受试者中,放射学确定的支气管扩张和支气管炎/细支气管炎明显更为常见(校正比值比= 2.9; 95%CI,2.0,4.3)。气道炎症受试者的HTLV-1c pVL中值比无症状受试者高16倍。在2,140人-年的随访中有151例死亡(最大随访8.13年)。死亡率以每10个HTLV-PVL 1C拷贝≥1000受试者中均高于5的外周血白细胞(对数秩χ 2(2DF)= 6.63,P = 0.036)相比,那些具有较低HTLV-PVL 1C或未感染的受试者。死亡率过高主要是由于支气管扩张相关的死亡(校正后的HR 4.31; 95%CI,1.78、10.42与未感染相比)。
结论/意义
较高的HTLV-1c pVL与放射学确定的气道炎症以及由于支气管扩张并发症导致的死亡密切相关。先前尚未证明由于HTLV-1相关的炎性疾病而增加的死亡风险。我们的发现表明,与HTLV-1c感染相关的死亡率可能高于以前的认识。需要进一步的前瞻性研究,以确定这些结果是否可以推广到其他HTLV-1流行地区。











































 京公网安备 11010802027423号
京公网安备 11010802027423号