Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Radical Prostatectomy, External Beam Radiotherapy, or External Beam Radiotherapy With Brachytherapy Boost and Disease Progression and Mortality in Patients With Gleason Score 9-10 Prostate Cancer
JAMA ( IF 63.1 ) Pub Date : 2018-03-06 , DOI: 10.1001/jama.2018.0587 Amar U. Kishan 1 , Ryan R. Cook 2 , Jay P. Ciezki 3 , Ashley E. Ross 4 , Mark M. Pomerantz 5 , Paul L. Nguyen 6 , Talha Shaikh 7 , Phuoc T. Tran 8 , Kiri A. Sandler 1 , Richard G. Stock 9 , Gregory S. Merrick 10 , D. Jeffrey Demanes 1 , Daniel E. Spratt 11 , Eyad I. Abu-Isa 11 , Trude B. Wedde 12 , Wolfgang Lilleby 12 , Daniel J. Krauss 13 , Grace K. Shaw 5 , Ridwan Alam 4 , Chandana A. Reddy 3 , Andrew J. Stephenson 14 , Eric A. Klein 14 , Daniel Y. Song 8 , Jeffrey J. Tosoian 4 , John V. Hegde 1 , Sun Mi Yoo 1 , Ryan Fiano 10 , Anthony V. D’Amico 6 , Nicholas G. Nickols 1, 15 , William J. Aronson 16 , Ahmad Sadeghi 15 , Stephen Greco 8 , Curtiland Deville 8 , Todd McNutt 8 , Theodore L. DeWeese 8 , Robert E. Reiter 16 , Johnathan W. Said 17 , Michael L. Steinberg 1 , Eric M. Horwitz 7 , Patrick A. Kupelian 1, 18 , Christopher R. King 1
JAMA ( IF 63.1 ) Pub Date : 2018-03-06 , DOI: 10.1001/jama.2018.0587 Amar U. Kishan 1 , Ryan R. Cook 2 , Jay P. Ciezki 3 , Ashley E. Ross 4 , Mark M. Pomerantz 5 , Paul L. Nguyen 6 , Talha Shaikh 7 , Phuoc T. Tran 8 , Kiri A. Sandler 1 , Richard G. Stock 9 , Gregory S. Merrick 10 , D. Jeffrey Demanes 1 , Daniel E. Spratt 11 , Eyad I. Abu-Isa 11 , Trude B. Wedde 12 , Wolfgang Lilleby 12 , Daniel J. Krauss 13 , Grace K. Shaw 5 , Ridwan Alam 4 , Chandana A. Reddy 3 , Andrew J. Stephenson 14 , Eric A. Klein 14 , Daniel Y. Song 8 , Jeffrey J. Tosoian 4 , John V. Hegde 1 , Sun Mi Yoo 1 , Ryan Fiano 10 , Anthony V. D’Amico 6 , Nicholas G. Nickols 1, 15 , William J. Aronson 16 , Ahmad Sadeghi 15 , Stephen Greco 8 , Curtiland Deville 8 , Todd McNutt 8 , Theodore L. DeWeese 8 , Robert E. Reiter 16 , Johnathan W. Said 17 , Michael L. Steinberg 1 , Eric M. Horwitz 7 , Patrick A. Kupelian 1, 18 , Christopher R. King 1
Affiliation
|
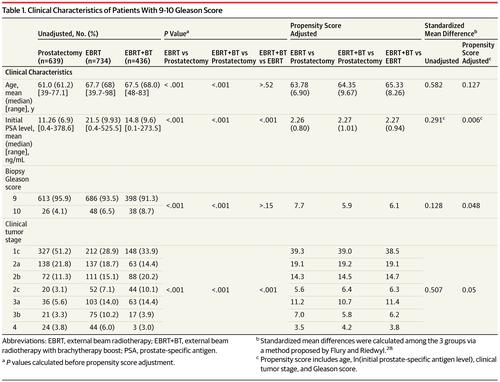
Importance The optimal treatment for Gleason score 9-10 prostate cancer is unknown. Objective To compare clinical outcomes of patients with Gleason score 9-10 prostate cancer after definitive treatment. Design, Setting, and Participants Retrospective cohort study in 12 tertiary centers (11 in the United States, 1 in Norway), with 1809 patients treated between 2000 and 2013. Exposures Radical prostatectomy (RP), external beam radiotherapy (EBRT) with androgen deprivation therapy, or EBRT plus brachytherapy boost (EBRT+BT) with androgen deprivation therapy. Main Outcomes and Measures The primary outcome was prostate cancer–specific mortality; distant metastasis-free survival and overall survival were secondary outcomes. Results Of 1809 men, 639 underwent RP, 734 EBRT, and 436 EBRT+BT. Median ages were 61, 67.7, and 67.5 years; median follow-up was 4.2, 5.1, and 6.3 years, respectively. By 10 years, 91 RP, 186 EBRT, and 90 EBRT+BT patients had died. Adjusted 5-year prostate cancer–specific mortality rates were RP, 12% (95% CI, 8%-17%); EBRT, 13% (95% CI, 8%-19%); and EBRT+BT, 3% (95% CI, 1%-5%). EBRT+BT was associated with significantly lower prostate cancer–specific mortality than either RP or EBRT (cause-specific HRs of 0.38 [95% CI, 0.21-0.68] and 0.41 [95% CI, 0.24-0.71]). Adjusted 5-year incidence rates of distant metastasis were RP, 24% (95% CI, 19%-30%); EBRT, 24% (95% CI, 20%-28%); and EBRT+BT, 8% (95% CI, 5%-11%). EBRT+BT was associated with a significantly lower rate of distant metastasis (propensity-score-adjusted cause-specific HRs of 0.27 [95% CI, 0.17-0.43] for RP and 0.30 [95% CI, 0.19-0.47] for EBRT). Adjusted 7.5-year all-cause mortality rates were RP, 17% (95% CI, 11%-23%); EBRT, 18% (95% CI, 14%-24%); and EBRT+BT, 10% (95% CI, 7%-13%). Within the first 7.5 years of follow-up, EBRT+BT was associated with significantly lower all-cause mortality (cause-specific HRs of 0.66 [95% CI, 0.46-0.96] for RP and 0.61 [95% CI, 0.45-0.84] for EBRT). After the first 7.5 years, the corresponding HRs were 1.16 (95% CI, 0.70-1.92) and 0.87 (95% CI, 0.57-1.32). No significant differences in prostate cancer–specific mortality, distant metastasis, or all-cause mortality (⩽7.5 and >7.5 years) were found between men treated with EBRT or RP (cause-specific HRs of 0.92 [95% CI, 0.67-1.26], 0.90 [95% CI, 0.70-1.14], 1.07 [95% CI, 0.80-1.44], and 1.34 [95% CI, 0.85-2.11]). Conclusions and Relevance Among patients with Gleason score 9-10 prostate cancer, treatment with EBRT+BT with androgen deprivation therapy was associated with significantly better prostate cancer–specific mortality and longer time to distant metastasis compared with EBRT with androgen deprivation therapy or with RP.
中文翻译:

Gleason 评分 9-10 前列腺癌患者的根治性前列腺切除术、外束放疗或外束放疗联合近距离放射治疗和疾病进展和死亡率
重要性 Gleason 评分 9-10 的前列腺癌的最佳治疗方法尚不清楚。目的 比较 Gleason 评分 9-10 分的前列腺癌患者根治性治疗后的临床结局。设计、设置和参与者 在 12 个三级中心(美国 11 个,挪威 1 个)进行的回顾性队列研究,在 2000 年至 2013 年间治疗了 1809 名患者。 暴露 根治性前列腺切除术 (RP)、外照射放疗 (EBRT) 和雄激素剥夺治疗,或 EBRT 加近距离放疗加强 (EBRT+BT) 和雄激素剥夺疗法。主要结果和措施 主要结果是前列腺癌特异性死亡率;无远处转移生存期和总生存期是次要结果。结果 在 1809 名男性中,639 人接受了 RP,734 人接受了 EBRT,436 人接受了 EBRT+BT。中位年龄分别为 61、67.7 和 67.5 岁;中位随访时间为 4。分别为 2、5.1 和 6.3 年。到 10 年时,91 名 RP、186 名 EBRT 和 90 名 EBRT+BT 患者死亡。调整后的 5 年前列腺癌特异性死亡率为 RP,12%(95% CI,8%-17%);EBRT,13%(95% CI,8%-19%);和 EBRT+BT,3%(95% CI,1%-5%)。EBRT+BT 与前列腺癌特异性死亡率显着低于 RP 或 EBRT 相关(原因特异性 HR 为 0.38 [95% CI,0.21-0.68] 和 0.41 [95% CI,0.24-0.71])。调整后的 5 年远处转移发生率为 RP,24%(95% CI,19%-30%);EBRT,24%(95% CI,20%-28%);和 EBRT+BT,8%(95% CI,5%-11%)。EBRT+BT 与远处转移率显着降低相关(RP 的倾向评分调整原因特异性 HR 为 0.27 [95% CI,0.17-0.43],EBRT 为 0.30 [95% CI,0.19-0.47]) . 调整后的 7.5 年全因死亡率为 RP,17%(95% CI,11%-23%);EBRT,18%(95% CI,14%-24%);和 EBRT+BT,10%(95% CI,7%-13%)。在随访的前 7.5 年中,EBRT+BT 与显着降低的全因死亡率相关(RP 的特定原因 HR 为 0.66 [95% CI,0.46-0.96] 和 0.61 [95% CI,0.45-0.84] ] 用于 EBRT)。在前 7.5 年之后,相应的 HR 分别为 1.16(95% CI,0.70-1.92)和 0.87(95% CI,0.57-1.32)。在接受 EBRT 或 RP 治疗的男性之间没有发现前列腺癌特异性死亡率、远处转移或全因死亡率(⩽7.5 和 >7.5 年)的显着差异(原因特异性 HR 为 0.92 [95% CI,0.67-1.26] ]、0.90 [95% CI,0.70-1.14]、1.07 [95% CI,0.80-1.44] 和 1.34 [95% CI,0.85-2.11])。结论和相关性 在 Gleason 评分为 9-10 的前列腺癌患者中,
更新日期:2018-03-06
中文翻译:

Gleason 评分 9-10 前列腺癌患者的根治性前列腺切除术、外束放疗或外束放疗联合近距离放射治疗和疾病进展和死亡率
重要性 Gleason 评分 9-10 的前列腺癌的最佳治疗方法尚不清楚。目的 比较 Gleason 评分 9-10 分的前列腺癌患者根治性治疗后的临床结局。设计、设置和参与者 在 12 个三级中心(美国 11 个,挪威 1 个)进行的回顾性队列研究,在 2000 年至 2013 年间治疗了 1809 名患者。 暴露 根治性前列腺切除术 (RP)、外照射放疗 (EBRT) 和雄激素剥夺治疗,或 EBRT 加近距离放疗加强 (EBRT+BT) 和雄激素剥夺疗法。主要结果和措施 主要结果是前列腺癌特异性死亡率;无远处转移生存期和总生存期是次要结果。结果 在 1809 名男性中,639 人接受了 RP,734 人接受了 EBRT,436 人接受了 EBRT+BT。中位年龄分别为 61、67.7 和 67.5 岁;中位随访时间为 4。分别为 2、5.1 和 6.3 年。到 10 年时,91 名 RP、186 名 EBRT 和 90 名 EBRT+BT 患者死亡。调整后的 5 年前列腺癌特异性死亡率为 RP,12%(95% CI,8%-17%);EBRT,13%(95% CI,8%-19%);和 EBRT+BT,3%(95% CI,1%-5%)。EBRT+BT 与前列腺癌特异性死亡率显着低于 RP 或 EBRT 相关(原因特异性 HR 为 0.38 [95% CI,0.21-0.68] 和 0.41 [95% CI,0.24-0.71])。调整后的 5 年远处转移发生率为 RP,24%(95% CI,19%-30%);EBRT,24%(95% CI,20%-28%);和 EBRT+BT,8%(95% CI,5%-11%)。EBRT+BT 与远处转移率显着降低相关(RP 的倾向评分调整原因特异性 HR 为 0.27 [95% CI,0.17-0.43],EBRT 为 0.30 [95% CI,0.19-0.47]) . 调整后的 7.5 年全因死亡率为 RP,17%(95% CI,11%-23%);EBRT,18%(95% CI,14%-24%);和 EBRT+BT,10%(95% CI,7%-13%)。在随访的前 7.5 年中,EBRT+BT 与显着降低的全因死亡率相关(RP 的特定原因 HR 为 0.66 [95% CI,0.46-0.96] 和 0.61 [95% CI,0.45-0.84] ] 用于 EBRT)。在前 7.5 年之后,相应的 HR 分别为 1.16(95% CI,0.70-1.92)和 0.87(95% CI,0.57-1.32)。在接受 EBRT 或 RP 治疗的男性之间没有发现前列腺癌特异性死亡率、远处转移或全因死亡率(⩽7.5 和 >7.5 年)的显着差异(原因特异性 HR 为 0.92 [95% CI,0.67-1.26] ]、0.90 [95% CI,0.70-1.14]、1.07 [95% CI,0.80-1.44] 和 1.34 [95% CI,0.85-2.11])。结论和相关性 在 Gleason 评分为 9-10 的前列腺癌患者中,











































 京公网安备 11010802027423号
京公网安备 11010802027423号