JAMA Surgery ( IF 15.7 ) Pub Date : 2018-02-01 , DOI: 10.1001/jamasurg.2017.3827 Elaine Vo 1 , Nader N Massarweh 1, 2, 3 , Christy Y Chai 1, 2 , Hop S Tran Cao 1, 2 , Nader Zamani 1 , Sherry Abraham 2 , Kafayat Adigun 2 , Samir S Awad 1, 2
|
Importance Surgical site infections (SSIs) after colorectal surgery remain a significant complication, particularly for patients with cancer, because they can delay the administration of adjuvant therapy. A combination of oral antibiotics and mechanical bowel preparation (MBP) is a potential, yet controversial, SSI prevention strategy.
Objective To determine the association of the addition of oral antibiotics to MBP with preventing SSIs in left colon and rectal cancer resections and its association with the timely administration of adjuvant therapy.
Design, Setting, and Participants A retrospective review was performed of 89 patients undergoing left colon and rectal cancer resections from October 1, 2013, to December 31, 2016, at a single institution. A bowel regimen of oral antibiotics and MBP (neomycin sulfate, metronidazole hydrochloride, and magnesium citrate) was implemented August 1, 2015. Patients receiving MBP and oral antibiotics and those undergoing MBP without oral antibiotics were compared using univariate analysis. Multivariable logistic regression controlling for factors that may affect SSIs was used to evaluate the association between use of oral antibiotics and MBP and the occurrence of SSIs.
Main Outcomes and Measures Surgical site infections within 30 days of the index procedure and time to adjuvant therapy.
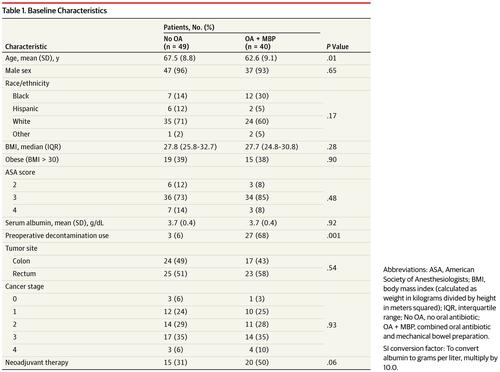
Results Of the 89 patients (5 women and 84 men; mean [SD] age, 65.3 [9.2] years) in the study, 49 underwent surgery with MBP but without oral antibiotics and 40 underwent surgery with MBP and oral antibiotics. The patients who received oral antibiotics and MBP were younger than those who received only MBP (mean [SD] age, 62.6 [9.1] vs 67.5 [8.8] years; P = .01), but these 2 cohorts of patients were otherwise similar in baseline demographic, clinical, and cancer characteristics. Surgical approach (minimally invasive vs open) and case type were similarly distributed; however, the median operative time of patients who received oral antibiotics and MBP was longer than that of patients who received MBP only (391 minutes [interquartile range, 302-550 minutes] vs 348 minutes [interquartile range, 248-425 minutes]; P = .03). The overall SSI rate was lower for patients who received oral antibiotics and MBP than for patients who received MBP only (3 [8%] vs 13 [27%]; P = .03), with no deep or organ space SSIs or anastomotic leaks in patients who received oral antibiotics and MBP compared with 9 organ space SSIs (18%; P = .004) and 5 anastomotic leaks (10%; P = .06) in patients who received MBP only. Despite this finding, there was no difference in median days to adjuvant therapy between the 2 cohorts (60 days [interquartile range, 46-73 days] for patients who received MBP only vs 72 days [interquartile range, 59-85 days] for patients who received oral antibiotics and MBP; P = .13). Oral antibiotics and MBP (odds ratio, 0.11; 95% CI, 0.02-0.86; P = .04) and minimally invasive surgery (odds ratio, 0.22; 95% CI, 0.05-0.89; P = .03) were independently associated with reduced odds of SSIs.
Conclusions and Relevance The combination of oral antibiotics and MBP is associated with a significant decrease in the rate of SSIs and should be considered for patients undergoing elective left colon and rectal cancer resections.
中文翻译:

左结肠癌和直肠癌切除术中在机械肠道准备中添加口服抗生素与减少手术部位感染的关系
结直肠手术后手术部位感染 (SSI) 的重要性 仍然是一个重要的并发症,特别是对于癌症患者,因为它们会延迟辅助治疗的实施。口服抗生素和机械肠道准备 (MBP) 的组合是一种潜在但有争议的 SSI 预防策略。
目的 确定在 MBP 中添加口服抗生素与预防左结肠癌和直肠癌切除术中 SSI 的关系及其与及时给予辅助治疗的关系。
设计、设置和参与者 对 2013 年 10 月 1 日至 2016 年 12 月 31 日在同一机构接受左结肠癌和直肠癌切除术的 89 名患者进行了回顾性研究。2015 年 8 月 1 日实施了口服抗生素和 MBP(硫酸新霉素、盐酸甲硝唑和柠檬酸镁)的肠道治疗方案。使用单变量分析比较了接受 MBP 和口服抗生素的患者与接受 MBP 而不口服抗生素的患者。控制可能影响 SSI 的因素的多变量逻辑回归用于评估口服抗生素和 MBP 的使用与 SSI 发生之间的关联。
主要结果和测量指标 手术后 30 天内的手术部位感染和辅助治疗时间。
结果 在研究中的 89 名患者(5 名女性和 84 名男性;平均 [SD] 年龄,65.3 [9.2] 岁)中,49 名接受了 MBP 手术但未使用口服抗生素,40 名患者接受了 MBP 和口服抗生素手术。接受口服抗生素和 MBP 的患者比仅接受 MBP 的患者年轻(平均 [SD] 年龄,62.6 [9.1] 对 67.5 [8.8] 岁;P = .01),但这两组患者在基线人口统计学、临床和癌症特征方面相似。手术方法(微创与开放)和病例类型分布相似;然而,接受口服抗生素和 MBP 的患者的中位手术时间长于仅接受 MBP 的患者(391 分钟 [四分位距,302-550 分钟] vs 348 分钟 [四分位距,248-425 分钟];P = .03)。接受口服抗生素和 MBP 的患者的总体 SSI 发生率低于仅接受 MBP 的患者(3 [8%] vs 13 [27%];P = .03),没有深部或器官空间 SSI 或吻合口漏在接受口服抗生素和 MBP 的患者中,与 9 个器官空间 SSI 相比(18%;P = .004) 和 5 例吻合口漏 (10%; P = .06) 仅接受 MBP 的患者。尽管有这一发现,但 2 个队列之间辅助治疗的中位天数没有差异(仅接受 MBP 的患者为 60 天 [四分位距,46-73 天],而仅接受 MBP 的患者为 72 天 [四分位距,59-85 天]接受口服抗生素和 MBP;P = .13)。口服抗生素和 MBP(优势比,0.11;95% CI,0.02-0.86;P = .04)和微创手术(优势比,0.22;95% CI,0.05-0.89;P = .03)独立相关降低 SSI 的几率。
结论和相关性 口服抗生素和 MBP 的组合与 SSI 发生率显着降低相关,应考虑用于接受选择性左结肠癌和直肠癌切除术的患者。











































 京公网安备 11010802027423号
京公网安备 11010802027423号