当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Outcome of ABO-incompatible adult living-donor liver transplantation for patients with hepatocellular carcinoma
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-02-13 , DOI: 10.1016/j.jhep.2018.02.002 Young-In Yoon , Gi-Won Song , Sung-Gyu Lee , Shin Hwang , Ki-Hun Kim , Seok-Hwan Kim , Woo-Hyoung Kang , Hwui-Dong Cho , Eun-Kyoung Jwa , Jae-Hyun Kwon , Eun-Young Tak , Varvara A. Kirchner
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-02-13 , DOI: 10.1016/j.jhep.2018.02.002 Young-In Yoon , Gi-Won Song , Sung-Gyu Lee , Shin Hwang , Ki-Hun Kim , Seok-Hwan Kim , Woo-Hyoung Kang , Hwui-Dong Cho , Eun-Kyoung Jwa , Jae-Hyun Kwon , Eun-Young Tak , Varvara A. Kirchner
|
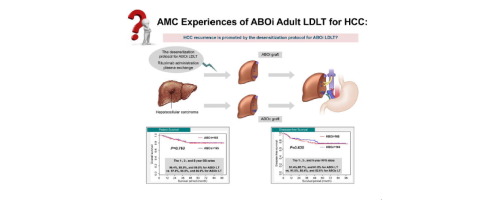
Living-donor liver transplantation (LDLT) can simultaneously cure hepatocellular carcinoma (HCC) and underlying liver cirrhosis, improving long-term results in patients with HCC. ABO-incompatible LDLT could expand the living-donor pool, reduce waiting times for deceased-donor liver transplantation, and improve long-term survival for some patients with HCC. We retrospectively reviewed the medical records of patients undergoing LDLT for HCC from November 2008 to December 2015 at a single institution in Korea. In total, 165 patients underwent ABO-incompatible and 753 patients underwent ABO-compatible LDLT for HCC. ABO-incompatible recipients underwent desensitization to overcome the ABO blood group barrier, including pretransplant plasma exchange and rituximab administration (300–375 mg/m /body surface area). We performed 1:1 propensity score matching and included 165 patients in each group. 82.4% of ABO-incompatible and 83.0% of -compatible LDLT groups had HCC within conventional Milan criteria, respectively, and 92.1% and 92.7% of patients in each group had a Child-Pugh score of A or B. ABO-incompatible and -compatible LDLT groups were followed up for 48.0 and 48.7 months, respectively, with both groups showing comparable recurrence-free survival rates (hazard ratio [HR] 1.14; 95% CI 0.68–1.90; = 0.630) and overall patient-survival outcomes (HR 1.10; 95% CI 0.60–2.00; = 0.763). These findings suggested that ABO-incompatible liver transplantation is a feasible option for patients with HCC, especially for those with compensated cirrhosis with HCC within conventional Milan criteria. Despite hypothetical immunological concerns that the desensitization protocol for breaking through the ABO blood group barrier might have a negative impact on the recurrence of hepatocellular carcinoma, our experience demonstrated no significant differences in the long-term overall survival and recurrence-free survival rates between patients receiving ABO-compatible or ABO-incompatible liver transplantation. In conclusion, results from our institution indicated that ABO-incompatible living-donor liver transplantation constitutes a potentially feasible option for patients with hepatocellular carcinoma, especially those with compensated cirrhosis with hepatocellular carcinoma within conventional Milan criteria.
中文翻译:

ABO血型不合成人活体肝移植治疗肝细胞癌的结果
活体肝移植(LDLT)可以同时治愈肝细胞癌(HCC)和潜在的肝硬化,改善HCC患者的长期疗效。 ABO 不相容的 LDLT 可以扩大活体供体库,减少死者供体肝移植的等待时间,并提高一些 HCC 患者的长期生存率。我们回顾性审查了 2008 年 11 月至 2015 年 12 月在韩国一家机构接受 LDLT 治疗 HCC 的患者的医疗记录。总共有 165 名患者接受了 ABO 不相容的 HCC 治疗,753 名患者接受了 ABO 相容的 LDLT。 ABO 血型不相容的受者接受脱敏治疗以克服 ABO 血型障碍,包括移植前血浆置换和利妥昔单抗给药(300-375 mg/m2/体表面积)。我们进行了 1:1 倾向评分匹配,每组包括 165 名患者。 ABO 血型不相容的 LDLT 组和 LDLT 相容的 LDLT 组中,分别有 82.4% 和 83.0% 的患者患有符合传统米兰标准的 HCC,每组中 92.1% 和 92.7% 的患者的 Child-Pugh 评分为 A 或 B。ABO 不相容和 -相容的 LDLT 组分别随访了 48.0 和 48.7 个月,两组均显示出相当的无复发生存率(风险比 [HR] 1.14;95% CI 0.68–1.90;= 0.630)和患者总体生存结果(HR) 1.10;95% CI 0.60-2.00;= 0.763)。这些发现表明,ABO 血型不合肝移植对于 HCC 患者来说是一种可行的选择,特别是对于那些符合传统米兰标准的代偿性肝硬化合并 HCC 的患者。尽管假设免疫学担心突破 ABO 血型屏障的脱敏方案可能对肝细胞癌的复发产生负面影响,但我们的经验表明,接受治疗的患者之间的长期总生存率和无复发生存率没有显着差异。 ABO 相容或 ABO 不相容肝移植。总之,我们机构的结果表明,ABO 血型不合的活体肝移植对于肝细胞癌患者,尤其是那些符合传统米兰标准的代偿性肝硬化肝细胞癌患者来说是一种潜在可行的选择。
更新日期:2018-02-13
中文翻译:

ABO血型不合成人活体肝移植治疗肝细胞癌的结果
活体肝移植(LDLT)可以同时治愈肝细胞癌(HCC)和潜在的肝硬化,改善HCC患者的长期疗效。 ABO 不相容的 LDLT 可以扩大活体供体库,减少死者供体肝移植的等待时间,并提高一些 HCC 患者的长期生存率。我们回顾性审查了 2008 年 11 月至 2015 年 12 月在韩国一家机构接受 LDLT 治疗 HCC 的患者的医疗记录。总共有 165 名患者接受了 ABO 不相容的 HCC 治疗,753 名患者接受了 ABO 相容的 LDLT。 ABO 血型不相容的受者接受脱敏治疗以克服 ABO 血型障碍,包括移植前血浆置换和利妥昔单抗给药(300-375 mg/m2/体表面积)。我们进行了 1:1 倾向评分匹配,每组包括 165 名患者。 ABO 血型不相容的 LDLT 组和 LDLT 相容的 LDLT 组中,分别有 82.4% 和 83.0% 的患者患有符合传统米兰标准的 HCC,每组中 92.1% 和 92.7% 的患者的 Child-Pugh 评分为 A 或 B。ABO 不相容和 -相容的 LDLT 组分别随访了 48.0 和 48.7 个月,两组均显示出相当的无复发生存率(风险比 [HR] 1.14;95% CI 0.68–1.90;= 0.630)和患者总体生存结果(HR) 1.10;95% CI 0.60-2.00;= 0.763)。这些发现表明,ABO 血型不合肝移植对于 HCC 患者来说是一种可行的选择,特别是对于那些符合传统米兰标准的代偿性肝硬化合并 HCC 的患者。尽管假设免疫学担心突破 ABO 血型屏障的脱敏方案可能对肝细胞癌的复发产生负面影响,但我们的经验表明,接受治疗的患者之间的长期总生存率和无复发生存率没有显着差异。 ABO 相容或 ABO 不相容肝移植。总之,我们机构的结果表明,ABO 血型不合的活体肝移植对于肝细胞癌患者,尤其是那些符合传统米兰标准的代偿性肝硬化肝细胞癌患者来说是一种潜在可行的选择。











































 京公网安备 11010802027423号
京公网安备 11010802027423号