JAMA Surgery ( IF 16.9 ) Pub Date : 2018-04-01 , DOI: 10.1001/jamasurg.2017.6112 Clara Nan-Hi Lee 1, 2, 3 , Michael Patrick Pignone 4, 5 , Allison M Deal 6 , Lillian Blizard 7 , Caprice Hunt 8 , Ruth Huh 6 , Yuen-Jong Liu 9 , Peter Anthony Ubel 5, 10, 11
|
Importance Making a good decision about breast reconstruction requires predicting how one would feel after the procedure, but people tend to overestimate the impact of events on future well-being.
Objective To assess how well patients predict future well-being after mastectomy, with or without immediate reconstruction, with the following a priori hypotheses: Patients will overestimate the negative impact of mastectomy and positive impact of reconstruction, and prediction accuracy will be associated with decision satisfaction and decision regret.
Design, Setting, and Participants This prospective cohort survey study was conducted at a single, multidisciplinary academic oncology clinic from July 2012 to February 2014. Adult women undergoing mastectomy for stage 1, 2, or 3 invasive ductal or lobular breast cancer, ductal carcinoma in situ, or prophylaxis were invited to participate. Data analysis was conducted from September 2015 to October 2017.
Exposures Mastectomy only or mastectomy with immediate reconstruction.
Main Outcomes and Measures Preoperative measures predicted were 12-month happiness (Cantril Ladder) and quality of life, predicted satisfaction with breasts, sexual attractiveness, breast numbness, and pain (measured with BreastQ single items). Measures at 12 months postoperative added the Decision Regret Scale and Satisfaction With Decisions Scale.
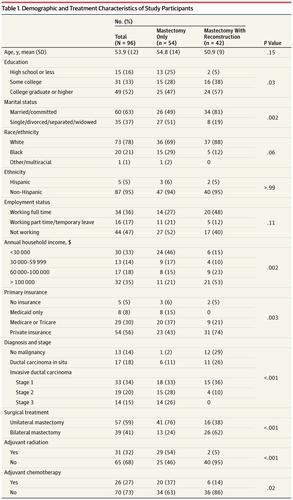
Results Of 214 eligible patients, 182 consecutive patients were approached, and 145 enrolled (80%). Of these 145 patients, 131 returned surveys (72%) and 111 of these remained at 12 months (88%). Fifteen who had delayed reconstruction were excluded from analysis, leaving a final cohort of 96 women; 54 had not had reconstruction and 42 had had reconstruction. The mean (SD) age of the cohort was 53.9 (12.1) years; 73 (76%) were white; 50 (52%) were college graduates; 54 (56%) were privately insured; 69 (72%) had disease at stages 0, 1, or 2; and 31 (32%) received adjuvant radiation. Patients having mastectomy without reconstruction underestimated future well-being in all domains. Differences were significant for quality of life scores (mean predicted, 68 vs mean actual, 74; t50, −2.47; P = .02) and satisfaction with breasts–clothed (mean predicted, 2.4 vs mean actual, 2.8; t49, −2.11; P = .04). Patients undergoing mastectomy with reconstruction overestimated future well-being in all but 1 domain. Differences were significant for satisfaction with breasts–unclothed (mean predicted, 3.1 vs mean actual, 2.6; t41, 2.70; P = .01); sexual attractiveness–clothed (mean predicted, 3.7 vs mean actual, 3.3; t39, 2.29; P = .03); sexual attractiveness–unclothed (mean predicted, 3.3 vs mean actual, 2.3; t40, 5.57; P < .001). Both groups experienced more numbness than predicted (mean predicted, 2.79 and 2.72 for mastectomy only and mastectomy with reconstruction groups, respectively; mean actual, 3.52 and 3.56, respectively; t47, −3.4 and t38, −2.9, respectively; P < .01). Patients who were less happy (β = 6.3; P = .02) or had greater pain (β = 8.7; P < .001) than predicted had greater regret.
Conclusions and Relevance Patients underestimated future well-being after mastectomy and overestimated well-being after reconstruction. Misprediction was associated with regret. Decision support for breast reconstruction should address expectations about well-being.
中文翻译:

即刻乳房重建术后乳腺癌患者未来健康预测的准确性
重要性 对乳房再造做出正确的决定需要预测手术后的感受,但人们往往会高估事件对未来幸福感的影响。
目的 评估患者在乳房切除术后(无论是否立即重建)对未来幸福感的预测程度,假设如下:患者会高估乳房切除术的负面影响和重建的积极影响,预测准确性与决策满意度相关和决定后悔。
设计、地点和参与者 这项前瞻性队列调查研究于 2012 年 7 月至 2014 年 2 月在一个单一的、多学科的学术肿瘤诊所进行。成年女性接受乳房切除术治疗 1、2 或 3 期浸润性导管或小叶乳腺癌、导管癌原位或预防被邀请参加。数据分析时间为 2015 年 9 月至 2017 年 10 月。
仅暴露 乳房切除术或乳房切除术并立即重建。
主要结果和 措施 预测的术前措施是 12 个月的幸福感(Cantril Ladder)和生活质量,预测的乳房满意度、性吸引力、乳房麻木和疼痛(用 BreastQ 单项测量)。术后 12 个月的测量增加了决策遗憾量表和决策满意度量表。
结果 在 214 名符合条件的患者中,连续接触了 182 名患者,其中 145 名(80%)入组。在这 145 名患者中,有 131 名返回调查(72%),其中 111 名保留在 12 个月(88%)。15 名延迟重建的患者被排除在分析之外,剩下的最终队列为 96 名女性;54 人未进行重建,42 人进行了重建。该队列的平均 (SD) 年龄为 53.9 (12.1) 岁;73 (76%) 人是白人;50 人(52%)是大学毕业生;54 (56%) 人参加了私人保险;69 人 (72%) 在 0、1 或 2 阶段患有疾病;31 人(32%)接受了辅助放疗。没有重建的乳房切除术患者低估了所有领域的未来福祉。生活质量评分差异显着(预测平均数 68 与实际平均数 74;t 50,-2.47;P = .02)和对穿着乳房的满意度(预测平均值 2.4 与实际平均值 2.8;t 49,-2.11;P = .04)。接受乳房切除术并重建的患者高估了除 1 个领域之外的所有未来幸福感。对裸露乳房的满意度差异显着(预测平均值为 3.1,实际平均值为 2.6;t 41,2.70;P = .01);性吸引力–穿着(平均预测,3.7 vs 平均实际,3.3;t 39,2.29;P = .03);性吸引力 - 不穿衣服(平均预测,3.3 vs 平均实际,2.3;t 40,5.57;P < .001)。两组都经历了比预期更多的麻木(仅乳房切除术组和乳房切除术重建组的平均预测值分别为 2.79 和 2.72;实际平均数分别为 3.52 和 3.56;t 47,-3.4 和t 38,-2.9;P < .01)。 比预期更不快乐(β = 6.3;P = .02)或疼痛更大(β = 8.7;P < .001)的患者后悔更大。
结论和相关性 患者低估了乳房切除术后的未来幸福感,而高估了重建后的幸福感。错误预测与后悔有关。乳房再造的决策支持应解决对健康的期望。



























 京公网安备 11010802027423号
京公网安备 11010802027423号