Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of Hysteroscopic vs Laparoscopic Sterilization With Procedural, Gynecological, and Medical Outcomes
JAMA ( IF 63.1 ) Pub Date : 2018-01-23 , DOI: 10.1001/jama.2017.21269 Kim Bouillon 1 , Marion Bertrand 1 , Georges Bader 2 , Jean-Philippe Lucot 3 , Rosemary Dray-Spira 1 , Mahmoud Zureik 1, 4
JAMA ( IF 63.1 ) Pub Date : 2018-01-23 , DOI: 10.1001/jama.2017.21269 Kim Bouillon 1 , Marion Bertrand 1 , Georges Bader 2 , Jean-Philippe Lucot 3 , Rosemary Dray-Spira 1 , Mahmoud Zureik 1, 4
Affiliation
|
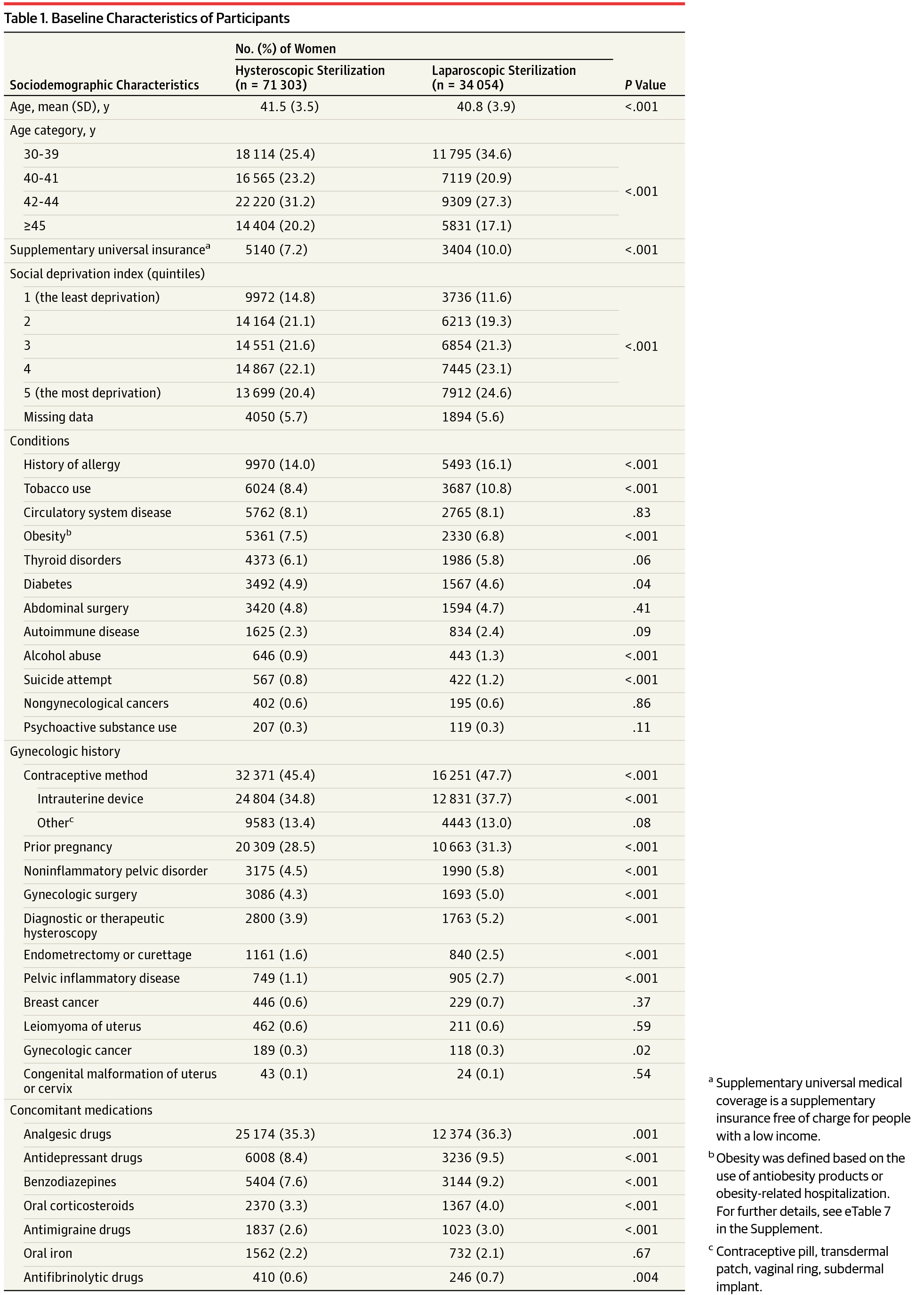
Importance Safety of hysteroscopic sterilization has been recently questioned following reports of general symptoms such as allergy, tiredness, and depression in addition to associated gynecological results such as pelvic pain, perforation of fallopian tubes or uterus, and unwanted pregnancy. Objective To compare the risk of reported adverse events between hysteroscopic and laparoscopic sterilization. Design, Setting, and Participants French nationwide cohort study using the national hospital discharge database linked to the health insurance claims database. Women aged 30 to 54 years receiving a first hysteroscopic or laparoscopic sterilization between 2010 and 2014 were included and were followed up through December 2015. Exposures Hysteroscopic sterilization vs laparoscopic sterilization. Main Outcomes and Measures Risks of procedural complications (surgical and medical) and of gynecological (sterilization failure that includes salpingectomy, second sterilization procedure, or pregnancy; pregnancy; reoperation) and medical outcomes (all types of allergy; autoimmune diseases; thyroid disorder; use of analgesics, antimigraines, antidepressants, benzodiazepines; outpatient visits; sickness absence; suicide attempts; death) that occurred within 1 and 3 years after sterilization were compared using inverse probability of treatment–weighted Cox models. Results Of the 105 357 women included (95.5% of eligible participants; mean age, 41.3 years [SD, 3.7 years]), 71 303 (67.7% ) underwent hysteroscopic sterilization, and 34 054 (32.3%) underwent laparoscopic sterilization. During the hospitalization for sterilization, risk of surgical complications for hysteroscopic sterilization was lower: 0.13% for hysteroscopic sterilization vs 0.78% for laparoscopic sterilization (adjusted risk difference [RD], −0.64; 95% CI, −0.67 to −0.60) and was lower for medical complications: 0.06% vs 0.11% (adjusted RD, −0.05; 95% CI, −0.08 to −0.01). During the first year after sterilization, 4.83% of women who underwent hysteroscopic sterilization had a higher risk of sterilization failure than the 0.69% who underwent laparoscopic sterilization (adjusted hazard ratio [HR], 7.11; 95% CI, 5.92 to 8.54; adjusted RD, 4.23 per 100 person-years; 95% CI, 3.40 to 5.22). Additionally, 5.65% of women who underwent hysteroscopic sterilization required gynecological reoperation vs 1.76% of women who underwent laparoscopic sterilization (adjusted HR, 3.26; 95% CI, 2.90 to 3.67; adjusted RD, 4.63 per 100 person-years; 95% CI, 3.38 to 4.75); these differences persisted after 3 years, although attenuated. Hysteroscopic sterilization was associated with a lower risk of pregnancy within the first year of the procedure but was not significantly associated with a difference in risk of pregnancy by the third year (adjusted HR, 1.04; 95% CI, 0.83-1.30; adjusted RD, 0.01 per 100 person-years; 95% CI, −0.04 to 0.07). Risks of medical outcomes were not significantly increased with hysteroscopic sterilization compared with laparoscopic sterilization. Conclusions and Relevance Among women undergoing first sterilization, the use of hysteroscopic sterilization was significantly associated with higher risk of gynecological complications over 1 year and over 3 years than was laparoscopic sterilization. Risk of medical outcomes was not significantly increased over 1 year or over 3 years. These findings do not support increased medical risks associated with hysteroscopic sterilization.
中文翻译:

宫腔镜与腹腔镜绝育与手术、妇科和医疗结果的关联
宫腔镜绝育的重要性最近在报告了过敏、疲倦和抑郁等一般症状以及相关的妇科结果(如骨盆疼痛、输卵管或子宫穿孔和意外怀孕)之后,安全性受到质疑。目的比较宫腔镜和腹腔镜绝育术之间报告的不良事件的风险。设计、设置和参与者法国全国队列研究使用与健康保险索赔数据库相关联的国家出院数据库。纳入 2010 年至 2014 年期间首次接受宫腔镜或腹腔镜绝育的 30 至 54 岁女性,并随访至 2015 年 12 月。 宫腔镜绝育与腹腔镜绝育的暴露。主要结果和措施 手术并发症(手术和医疗)和妇科(绝育失败,包括输卵管切除术、二次绝育手术或怀孕;怀孕;再次手术)和医疗结果(所有类型的过敏;自身免疫性疾病;甲状腺疾病;使用)的风险使用治疗加权 Cox 模型的逆概率比较了绝育后 1 年和 3 年内发生的镇痛药、抗偏头痛药、抗抑郁药、苯二氮卓类药物;门诊就诊;病假;自杀未遂;死亡)。结果 在纳入的 105 357 名女性中(符合条件的参与者的 95.5%;平均年龄为 41.3 岁 [SD,3.7 岁]),71 303 名(67.7%)接受了宫腔镜绝育术,34 054 名(32.3%)接受了腹腔镜绝育术。住院绝育期间,宫腔镜绝育手术并发症的风险较低:宫腔镜绝育为 0.13%,腹腔镜绝育为 0.78%(调整后风险差 [RD],-0.64;95% CI,-0.67 至 -0.60),医疗并发症风险更低:0.06 % 与 0.11%(调整后的 RD,-0.05;95% CI,-0.08 至 -0.01)。在绝育后的第一年,4.83% 接受宫腔镜绝育手术的女性绝育失败风险高于接受腹腔镜绝育手术的 0.69%(调整后的风险比 [HR],7.11;95% CI,5.92 至 8.54;调整后的 RD) ,每 100 人年 4.23;95% CI,3.40 至 5.22)。此外,5.65% 的接受宫腔镜绝育术的女性需要再次手术,而接受腹腔镜绝育术的女性为 1.76%(调整后的 HR,3.26;95% CI,2.90 至 3.67;调整后的 RD,4。每 100 人年 63 人;95% CI,3.38 至 4.75);这些差异在 3 年后仍然存在,但有所减弱。宫腔镜绝育术与手术第一年内较低的妊娠风险相关,但与第三年的妊娠风险差异无显着相关性(调整后的 HR,1.04;95% CI,0.83-1.30;调整后的 RD,每 100 人年 0.01;95% CI,-0.04 至 0.07)。与腹腔镜绝育相比,宫腔镜绝育的医疗结果风险并未显着增加。结论和相关性 在首次接受绝育手术的女性中,宫腔镜绝育术的使用与 1 年和 3 年以上妇科并发症的风险显着相关,而不是腹腔镜绝育术。医疗结果的风险在 1 年或 3 年内没有显着增加。这些发现不支持与宫腔镜绝育相关的医疗风险增加。
更新日期:2018-01-23
中文翻译:

宫腔镜与腹腔镜绝育与手术、妇科和医疗结果的关联
宫腔镜绝育的重要性最近在报告了过敏、疲倦和抑郁等一般症状以及相关的妇科结果(如骨盆疼痛、输卵管或子宫穿孔和意外怀孕)之后,安全性受到质疑。目的比较宫腔镜和腹腔镜绝育术之间报告的不良事件的风险。设计、设置和参与者法国全国队列研究使用与健康保险索赔数据库相关联的国家出院数据库。纳入 2010 年至 2014 年期间首次接受宫腔镜或腹腔镜绝育的 30 至 54 岁女性,并随访至 2015 年 12 月。 宫腔镜绝育与腹腔镜绝育的暴露。主要结果和措施 手术并发症(手术和医疗)和妇科(绝育失败,包括输卵管切除术、二次绝育手术或怀孕;怀孕;再次手术)和医疗结果(所有类型的过敏;自身免疫性疾病;甲状腺疾病;使用)的风险使用治疗加权 Cox 模型的逆概率比较了绝育后 1 年和 3 年内发生的镇痛药、抗偏头痛药、抗抑郁药、苯二氮卓类药物;门诊就诊;病假;自杀未遂;死亡)。结果 在纳入的 105 357 名女性中(符合条件的参与者的 95.5%;平均年龄为 41.3 岁 [SD,3.7 岁]),71 303 名(67.7%)接受了宫腔镜绝育术,34 054 名(32.3%)接受了腹腔镜绝育术。住院绝育期间,宫腔镜绝育手术并发症的风险较低:宫腔镜绝育为 0.13%,腹腔镜绝育为 0.78%(调整后风险差 [RD],-0.64;95% CI,-0.67 至 -0.60),医疗并发症风险更低:0.06 % 与 0.11%(调整后的 RD,-0.05;95% CI,-0.08 至 -0.01)。在绝育后的第一年,4.83% 接受宫腔镜绝育手术的女性绝育失败风险高于接受腹腔镜绝育手术的 0.69%(调整后的风险比 [HR],7.11;95% CI,5.92 至 8.54;调整后的 RD) ,每 100 人年 4.23;95% CI,3.40 至 5.22)。此外,5.65% 的接受宫腔镜绝育术的女性需要再次手术,而接受腹腔镜绝育术的女性为 1.76%(调整后的 HR,3.26;95% CI,2.90 至 3.67;调整后的 RD,4。每 100 人年 63 人;95% CI,3.38 至 4.75);这些差异在 3 年后仍然存在,但有所减弱。宫腔镜绝育术与手术第一年内较低的妊娠风险相关,但与第三年的妊娠风险差异无显着相关性(调整后的 HR,1.04;95% CI,0.83-1.30;调整后的 RD,每 100 人年 0.01;95% CI,-0.04 至 0.07)。与腹腔镜绝育相比,宫腔镜绝育的医疗结果风险并未显着增加。结论和相关性 在首次接受绝育手术的女性中,宫腔镜绝育术的使用与 1 年和 3 年以上妇科并发症的风险显着相关,而不是腹腔镜绝育术。医疗结果的风险在 1 年或 3 年内没有显着增加。这些发现不支持与宫腔镜绝育相关的医疗风险增加。











































 京公网安备 11010802027423号
京公网安备 11010802027423号