PLOS Medicine ( IF 10.5 ) Pub Date : 2018-01-16 , DOI: 10.1371/journal.pmed.1002492 Olufemi T Oladapo 1 , Joao Paulo Souza 1 , Bukola Fawole 2 , Kidza Mugerwa 3 , Gleici Perdoná 4 , Domingos Alves 4 , Hayala Souza 4 , Rodrigo Reis 4 , Livia Oliveira-Ciabati 4 , Alexandre Maiorano 5 , Adesina Akintan 6 , Francis E Alu 7 , Lawal Oyeneyin 8 , Amos Adebayo 9 , Josaphat Byamugisha 3 , Miriam Nakalembe 3 , Hadiza A Idris 10 , Ola Okike 11 , Fernando Althabe 12 , Vanora Hundley 13 , France Donnay 14 , Robert Pattinson 15 , Harshadkumar C Sanghvi 16 , Jen E Jardine 17 , Özge Tunçalp 1 , Joshua P Vogel 1 , Mary Ellen Stanton 18 , Meghan Bohren 1 , Jun Zhang 19 , Tina Lavender 20 , Jerker Liljestrand 21 , Petra Ten Hoope-Bender 22 , Matthews Mathai 23, 24 , Rajiv Bahl 23 , A Metin Gülmezoglu 1
|
Background
Escalation in the global rates of labour interventions, particularly cesarean section and oxytocin augmentation, has renewed interest in a better understanding of natural labour progression. Methodological advancements in statistical and computational techniques addressing the limitations of pioneer studies have led to novel findings and triggered a re-evaluation of current labour practices. As part of the World Health Organization's Better Outcomes in Labour Difficulty (BOLD) project, which aimed to develop a new labour monitoring-to-action tool, we examined the patterns of labour progression as depicted by cervical dilatation over time in a cohort of women in Nigeria and Uganda who gave birth vaginally following a spontaneous labour onset.
Methods and findings
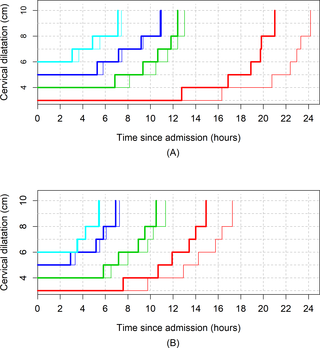
This was a prospective, multicentre, cohort study of 5,606 women with singleton, vertex, term gestation who presented at ≤ 6 cm of cervical dilatation following a spontaneous labour onset that resulted in a vaginal birth with no adverse birth outcomes in 13 hospitals across Nigeria and Uganda. We independently applied survival analysis and multistate Markov models to estimate the duration of labour centimetre by centimetre until 10 cm and the cumulative duration of labour from the cervical dilatation at admission through 10 cm. Multistate Markov and nonlinear mixed models were separately used to construct average labour curves. All analyses were conducted according to three parity groups: parity = 0 (n = 2,166), parity = 1 (n = 1,488), and parity = 2+ (n = 1,952). We performed sensitivity analyses to assess the impact of oxytocin augmentation on labour progression by re-examining the progression patterns after excluding women with augmented labours. Labour was augmented with oxytocin in 40% of nulliparous and 28% of multiparous women. The median time to advance by 1 cm exceeded 1 hour until 5 cm was reached in both nulliparous and multiparous women. Based on a 95th percentile threshold, nulliparous women may take up to 7 hours to progress from 4 to 5 cm and over 3 hours to progress from 5 to 6 cm. Median cumulative duration of labour indicates that nulliparous women admitted at 4 cm, 5 cm, and 6 cm reached 10 cm within an expected time frame if the dilatation rate was ≥ 1 cm/hour, but their corresponding 95th percentiles show that labour could last up to 14, 11, and 9 hours, respectively. Substantial differences exist between actual plots of labour progression of individual women and the ‘average labour curves’ derived from study population-level data. Exclusion of women with augmented labours from the study population resulted in slightly faster labour progression patterns.
Conclusions
Cervical dilatation during labour in the slowest-yet-normal women can progress more slowly than the widely accepted benchmark of 1 cm/hour, irrespective of parity. Interventions to expedite labour to conform to a cervical dilatation threshold of 1 cm/hour may be inappropriate, especially when applied before 5 cm in nulliparous and multiparous women. Averaged labour curves may not truly reflect the variability associated with labour progression, and their use for decision-making in labour management should be de-emphasized.
中文翻译:

第一阶段自然分娩的进展:两个撒哈拉以南非洲国家的前瞻性队列研究
背景
全球分娩干预率的上升,特别是剖腹产和催产素增强,重新激发了人们对更好地理解自然分娩进展的兴趣。统计和计算技术的方法论进步解决了先驱研究的局限性,带来了新的发现,并引发了对当前劳动实践的重新评估。作为世界卫生组织“更好的分娩困难结果”(BOLD) 项目的一部分,该项目旨在开发一种新的分娩监测行动工具,我们检查了一组妇女随时间推移宫颈扩张所描述的分娩进展模式。在尼日利亚和乌干达,她们在自然分娩后进行了阴道分娩。
方法和结果
这是一项前瞻性、多中心、队列研究,研究对象为 5,606 名单胎、顶角、足月妊娠妇女,她们在自然临产后宫颈扩张 ≤ 6 厘米,在尼日利亚和尼日利亚的 13 家医院进行了阴道分娩,没有出现不良分娩结果。乌干达。我们独立应用生存分析和多态马尔可夫模型来逐厘米估计产程持续时间,直到 10 厘米,以及从入院时宫颈扩张到 10 厘米的累积产程持续时间。分别采用多态马尔可夫模型和非线性混合模型构建平均劳动曲线。所有分析均根据三个胎次组进行:胎次 = 0 ( n = 2,166)、胎次 = 1 ( n = 1,488) 和胎次 = 2+ ( n = 1,952)。我们进行了敏感性分析,通过在排除增强产程的女性后重新检查进展模式来评估催产素增强对产程进展的影响。催产素对 40% 的未产妇和 28% 的经产妇增加了产程。未产妇和经产妇中,前进 1 厘米的中位时间超过 1 小时,直到达到 5 厘米。根据第 95 个百分位数阈值,未生育的女性可能需要长达 7 小时才能从 4 厘米长到 5 厘米,从 5 厘米长到 6 厘米可能需要 3 个小时以上。中位累积产程表明,如果宫缩率≥1厘米/小时,在4厘米、5厘米和6厘米入院的未产妇在预期时间范围内达到10厘米,但其相应的第95个百分位数表明产程可以持续分别为 14、11 和 9 小时。 个别妇女的实际产程进展图与从研究人口水平数据得出的“平均产程曲线”之间存在显着差异。将增加产程的女性排除在研究人群之外会导致产程进展模式稍快一些。
结论
无论胎次如何,最慢但正常的女性在分娩过程中的宫颈扩张速度可能会比广泛接受的 1 厘米/小时的基准更慢。加速分娩以符合 1 厘米/小时的宫颈扩张阈值的干预措施可能是不合适的,特别是在未产妇和多产妇女中实施 5 厘米之前的干预措施。平均劳动力曲线可能无法真正反映与劳动力进展相关的变异性,并且不应强调它们在劳动力管理决策中的应用。











































 京公网安备 11010802027423号
京公网安备 11010802027423号