Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients With Morbid Obesity
JAMA ( IF 63.1 ) Pub Date : 2018-01-16 , DOI: 10.1001/jama.2017.20897 Ralph Peterli 1 , Bettina Karin Wölnerhanssen 2, 3 , Thomas Peters 4 , Diana Vetter 5 , Dino Kröll 6 , Yves Borbély 6 , Bernd Schultes 7 , Christoph Beglinger 2 , Jürgen Drewe 8 , Marc Schiesser 9 , Philipp Nett 6 , Marco Bueter 5
JAMA ( IF 63.1 ) Pub Date : 2018-01-16 , DOI: 10.1001/jama.2017.20897 Ralph Peterli 1 , Bettina Karin Wölnerhanssen 2, 3 , Thomas Peters 4 , Diana Vetter 5 , Dino Kröll 6 , Yves Borbély 6 , Bernd Schultes 7 , Christoph Beglinger 2 , Jürgen Drewe 8 , Marc Schiesser 9 , Philipp Nett 6 , Marco Bueter 5
Affiliation
|
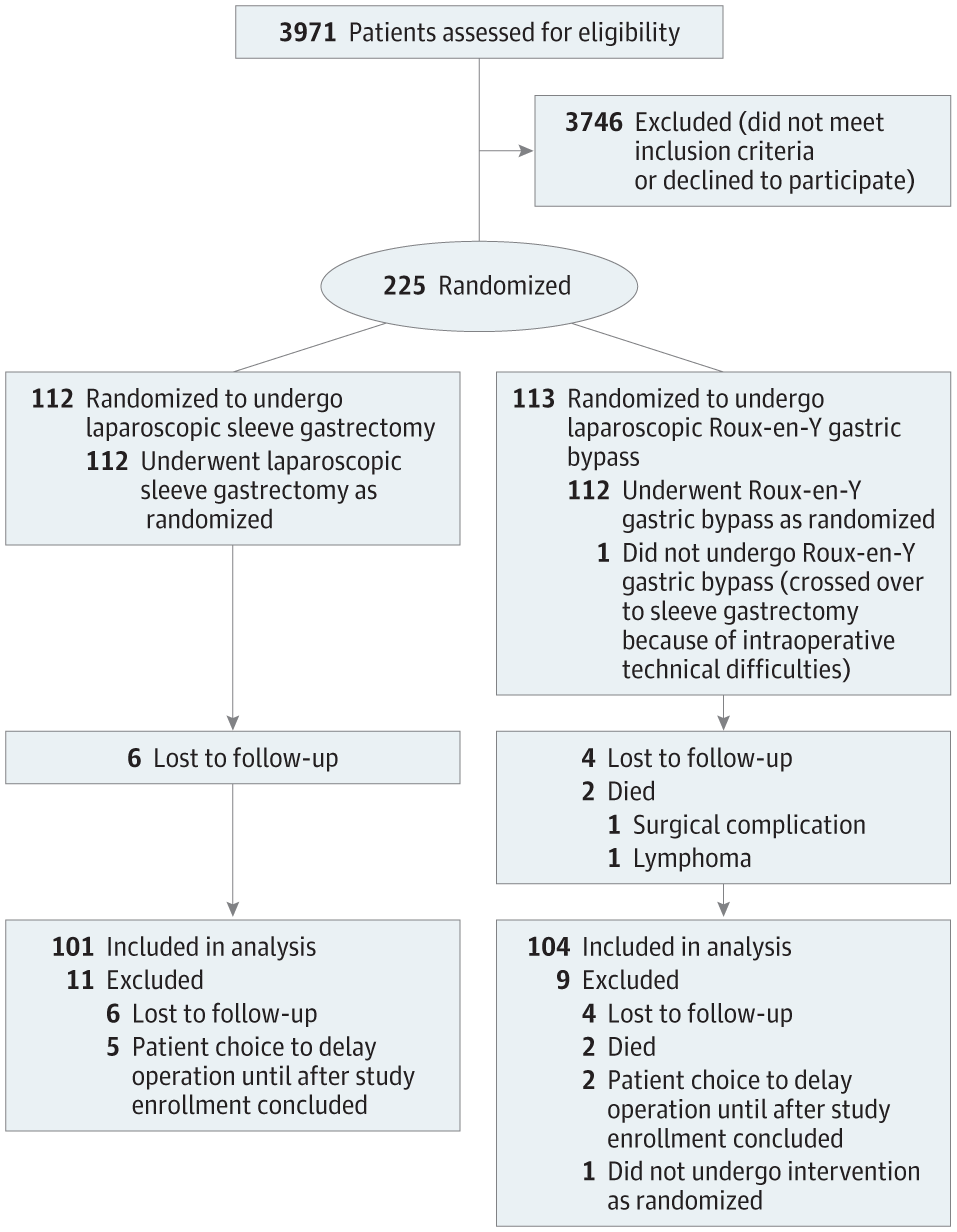
Importance Sleeve gastrectomy is increasingly used in the treatment of morbid obesity, but its long-term outcome vs the standard Roux-en-Y gastric bypass procedure is unknown. Objective To determine whether there are differences between sleeve gastrectomy and Roux-en-Y gastric bypass in terms of weight loss, changes in comorbidities, increase in quality of life, and adverse events. Design, Setting, and Participants The Swiss Multicenter Bypass or Sleeve Study (SM-BOSS), a 2-group randomized trial, was conducted from January 2007 until November 2011 (last follow-up in March 2017). Of 3971 morbidly obese patients evaluated for bariatric surgery at 4 Swiss bariatric centers, 217 patients were enrolled and randomly assigned to sleeve gastrectomy or Roux-en-Y gastric bypass with a 5-year follow-up period. Interventions Patients were randomly assigned to undergo laparoscopic sleeve gastrectomy (n = 107) or laparoscopic Roux-en-Y gastric bypass (n = 110). Main Outcomes and Measures The primary end point was weight loss, expressed as percentage excess body mass index (BMI) loss. Exploratory end points were changes in comorbidities and adverse events. Results Among the 217 patients (mean age, 45.5 years; 72% women; mean BMI, 43.9) 205 (94.5%) completed the trial. Excess BMI loss was not significantly different at 5 years: for sleeve gastrectomy, 61.1%, vs Roux-en-Y gastric bypass, 68.3% (absolute difference, −7.18%; 95% CI, −14.30% to −0.06%; P = .22 after adjustment for multiple comparisons). Gastric reflux remission was observed more frequently after Roux-en-Y gastric bypass (60.4%) than after sleeve gastrectomy (25.0%). Gastric reflux worsened (more symptoms or increase in therapy) more often after sleeve gastrectomy (31.8%) than after Roux-en-Y gastric bypass (6.3%). The number of patients with reoperations or interventions was 16/101 (15.8%) after sleeve gastrectomy and 23/104 (22.1%) after Roux-en-Y gastric bypass. Conclusions and Relevance Among patients with morbid obesity, there was no significant difference in excess BMI loss between laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass at 5 years of follow-up after surgery. Trial Registration clinicaltrials.gov Identifier: NCT00356213
中文翻译:

腹腔镜袖状胃切除术与腹腔镜 Roux-en-Y 胃绕道术对病态肥胖患者体重减轻的影响
重要性 袖状胃切除术越来越多地用于治疗病态肥胖,但其长期结果与标准 Roux-en-Y 胃绕道手术相比尚不清楚。目的 确定袖状胃切除术与 Roux-en-Y 胃旁路术在体重减轻、合并症变化、生活质量提高和不良事件方面是否存在差异。设计、设置和参与者 瑞士多中心旁路或套管研究 (SM-BOSS) 是一项 2 组随机试验,于 2007 年 1 月至 2011 年 11 月进行(最后一次随访于 2017 年 3 月)。在 4 个瑞士减肥中心接受减肥手术评估的 3971 名病态肥胖患者中,217 名患者被纳入并随机分配接受袖状胃切除术或 Roux-en-Y 胃旁路术,随访 5 年。干预 患者被随机分配接受腹腔镜袖状胃切除术(n = 107)或腹腔镜 Roux-en-Y 胃旁路术(n = 110)。主要结果和措施 主要终点是体重减轻,表示为体重指数 (BMI) 损失的百分比。探索性终点是合并症和不良事件的变化。结果 在 217 名患者(平均年龄 45.5 岁;72% 女性;平均 BMI 43.9)中,205 名(94.5%)完成了试验。5 年时过度 BMI 损失没有显着差异:袖状胃切除术,61.1%,与 Roux-en-Y 胃旁路术相比,68.3%(绝对差异,-7.18%;95% CI,-14.30% 至 -0.06%;P = .22 多重比较调整后)。Roux-en-Y 胃绕道手术后胃反流缓解率 (60.4%) 比袖状胃切除术后 (25.0%) 更频繁。与 Roux-en-Y 胃绕道手术(6.3%)相比,袖状胃切除术(31.8%)后胃反流恶化(更多症状或治疗增加)的频率更高。袖状胃切除术后再次手术或干预的患者人数为 16/101 (15.8%),Roux-en-Y 胃旁路手术后再次手术或干预的患者人数为 23/104 (22.1%)。结论和相关性 在病态肥胖患者中,腹腔镜袖状胃切除术和腹腔镜 Roux-en-Y 胃绕道术在术后 5 年随访中的超量 BMI 损失没有显着差异。试验注册clinicaltrials.gov 标识符:NCT00356213 1%) Roux-en-Y 胃绕道手术后。结论和相关性 在病态肥胖患者中,腹腔镜袖状胃切除术和腹腔镜 Roux-en-Y 胃绕道术在术后 5 年随访中的超量 BMI 损失没有显着差异。试验注册clinicaltrials.gov 标识符:NCT00356213 1%) Roux-en-Y 胃绕道手术后。结论和相关性 在病态肥胖患者中,腹腔镜袖状胃切除术和腹腔镜 Roux-en-Y 胃绕道术在术后 5 年随访中的超量 BMI 损失没有显着差异。试验注册clinicaltrials.gov 标识符:NCT00356213
更新日期:2018-01-16
中文翻译:

腹腔镜袖状胃切除术与腹腔镜 Roux-en-Y 胃绕道术对病态肥胖患者体重减轻的影响
重要性 袖状胃切除术越来越多地用于治疗病态肥胖,但其长期结果与标准 Roux-en-Y 胃绕道手术相比尚不清楚。目的 确定袖状胃切除术与 Roux-en-Y 胃旁路术在体重减轻、合并症变化、生活质量提高和不良事件方面是否存在差异。设计、设置和参与者 瑞士多中心旁路或套管研究 (SM-BOSS) 是一项 2 组随机试验,于 2007 年 1 月至 2011 年 11 月进行(最后一次随访于 2017 年 3 月)。在 4 个瑞士减肥中心接受减肥手术评估的 3971 名病态肥胖患者中,217 名患者被纳入并随机分配接受袖状胃切除术或 Roux-en-Y 胃旁路术,随访 5 年。干预 患者被随机分配接受腹腔镜袖状胃切除术(n = 107)或腹腔镜 Roux-en-Y 胃旁路术(n = 110)。主要结果和措施 主要终点是体重减轻,表示为体重指数 (BMI) 损失的百分比。探索性终点是合并症和不良事件的变化。结果 在 217 名患者(平均年龄 45.5 岁;72% 女性;平均 BMI 43.9)中,205 名(94.5%)完成了试验。5 年时过度 BMI 损失没有显着差异:袖状胃切除术,61.1%,与 Roux-en-Y 胃旁路术相比,68.3%(绝对差异,-7.18%;95% CI,-14.30% 至 -0.06%;P = .22 多重比较调整后)。Roux-en-Y 胃绕道手术后胃反流缓解率 (60.4%) 比袖状胃切除术后 (25.0%) 更频繁。与 Roux-en-Y 胃绕道手术(6.3%)相比,袖状胃切除术(31.8%)后胃反流恶化(更多症状或治疗增加)的频率更高。袖状胃切除术后再次手术或干预的患者人数为 16/101 (15.8%),Roux-en-Y 胃旁路手术后再次手术或干预的患者人数为 23/104 (22.1%)。结论和相关性 在病态肥胖患者中,腹腔镜袖状胃切除术和腹腔镜 Roux-en-Y 胃绕道术在术后 5 年随访中的超量 BMI 损失没有显着差异。试验注册clinicaltrials.gov 标识符:NCT00356213 1%) Roux-en-Y 胃绕道手术后。结论和相关性 在病态肥胖患者中,腹腔镜袖状胃切除术和腹腔镜 Roux-en-Y 胃绕道术在术后 5 年随访中的超量 BMI 损失没有显着差异。试验注册clinicaltrials.gov 标识符:NCT00356213 1%) Roux-en-Y 胃绕道手术后。结论和相关性 在病态肥胖患者中,腹腔镜袖状胃切除术和腹腔镜 Roux-en-Y 胃绕道术在术后 5 年随访中的超量 BMI 损失没有显着差异。试验注册clinicaltrials.gov 标识符:NCT00356213











































 京公网安备 11010802027423号
京公网安备 11010802027423号