Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Estimated mortality on HIV treatment among active patients and patients lost to follow-up in 4 provinces of Zambia: Findings from a multistage sampling-based survey.
PLOS Medicine ( IF 10.5 ) Pub Date : 2018-01-12 , DOI: 10.1371/journal.pmed.1002489 Charles B Holmes 1, 2, 3 , Izukanji Sikazwe 1 , Kombatende Sikombe 1 , Ingrid Eshun-Wilson 4 , Nancy Czaicki 1, 5 , Laura K Beres 2 , Njekwa Mukamba 1 , Sandra Simbeza 1 , Carolyn Bolton Moore 1, 6 , Cardinal Hantuba 1 , Peter Mwaba 7 , Caroline Phiri 8 , Nancy Padian 5 , David V Glidden 9 , Elvin Geng 9
PLOS Medicine ( IF 10.5 ) Pub Date : 2018-01-12 , DOI: 10.1371/journal.pmed.1002489 Charles B Holmes 1, 2, 3 , Izukanji Sikazwe 1 , Kombatende Sikombe 1 , Ingrid Eshun-Wilson 4 , Nancy Czaicki 1, 5 , Laura K Beres 2 , Njekwa Mukamba 1 , Sandra Simbeza 1 , Carolyn Bolton Moore 1, 6 , Cardinal Hantuba 1 , Peter Mwaba 7 , Caroline Phiri 8 , Nancy Padian 5 , David V Glidden 9 , Elvin Geng 9
Affiliation
|
BACKGROUND
Survival represents the single most important indicator of successful HIV treatment. Routine monitoring fails to capture most deaths. As a result, both regional assessments of the impact of HIV services and identification of hotspots for improvement efforts are limited. We sought to assess true mortality on treatment, characterize the extent under-reporting of mortality in routine health information systems in Zambia, and identify drivers of mortality across sites and over time using a multistage, regionally representative sampling approach.
METHODS AND FINDINGS
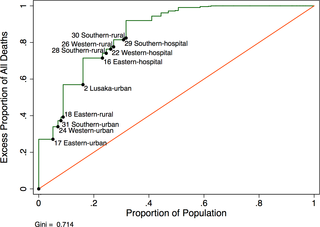
We enumerated all HIV infected adults on antiretroviral therapy (ART) who visited any one of 64 facilities across 4 provinces in Zambia during the 24-month period from 1 August 2013 to 31 July 2015. We identified a probability sample of patients who were lost to follow-up through selecting facilities probability proportional to size and then a simple random sample of lost patients. Outcomes among patients lost to follow-up were incorporated into survival analysis and multivariate regression through probability weights. Of 165,464 individuals (64% female, median age 39 years (IQR 33-46), median CD4 201 cells/mm3 (IQR 111-312), the 2-year cumulative incidence of mortality increased from 1.9% (95% CI 1.7%-2.0%) to a corrected rate of 7.0% (95% CI 5.7%-8.4%) (all ART users) and from 2.1% (95% CI 1.8%-2.4%) to 8.3% (95% CI 6.1%-10.7%) (new ART users). Revised provincial mortality rates ranged from 3-9 times higher than naïve rates for new ART users and were lowest in Lusaka Province (4.6 per 100 person-years) and highest in Western Province (8.7 per 100 person-years) after correction. Corrected mortality rates varied markedly by clinic, with an IQR of 3.5 to 7.5 deaths per 100 person-years and a high of 13.4 deaths per 100 person-years among new ART users, even after adjustment for clinical (e.g., pretherapy CD4) and contextual (e.g., province and clinic size) factors. Mortality rates (all ART users) were highest year 1 after treatment at 4.6/100 person-years (95% CI 3.9-5.5), 2.9/100 person-years (95% CI 2.1-3.9) in year 2, and approximately 1.6% per year through 8 years on treatment. In multivariate analysis, patient-level factors including male sex and pretherapy CD4 levels and WHO stage were associated with higher mortality among new ART users, while male sex and HIV disclosure were associated with mortality among all ART users. In both cases, being late (>14 days late for appointment) or lost (>90 days late for an appointment) was associated with deaths. We were unable to ascertain the vital status of about one-quarter of those lost and selected for tracing and did not adjudicate causes of death.
CONCLUSIONS
HIV treatment in Zambia is not optimally effective. The high and sustained mortality rates and marked under-reporting of mortality at the provincial-level and unexplained heterogeneity between regions and sites suggest opportunities for the use of corrected mortality rates for quality improvement. A regionally representative sampling-based approach can bring gaps and opportunities for programs into clear epidemiological focus for local and global decision makers.
中文翻译:

在赞比亚4个省中,活跃患者和失去随访的患者中HIV治疗的估计死亡率:基于多阶段抽样调查的结果。
背景技术存活率是成功治疗HIV的最重要的单一指标。例行监测未能捕获大多数死亡。结果,对艾滋病毒服务影响的区域评估和为改进工作而确定的热点都受到限制。我们试图评估治疗中的真实死亡率,表征赞比亚常规卫生信息系统中死亡率低报的程度,并使用多阶段,地区代表性的抽样方法确定各地间和一段时间内的死亡率驱动因素。方法和研究结果我们列举了所有接受抗逆转录病毒疗法(ART)感染HIV的成年人,他们在2013年8月1日至2015年7月31日的24个月内访问了赞比亚4个省的64个设施中的任何一个。通过选择与规模成正比的设施概率,然后选择一个简单的随机丢失患者样本,我们确定了丢失随访患者的概率样本。失去随访的患者的结果通过概率加权纳入生存分析和多元回归。在165,464个人中(64%女性,中位年龄39岁(IQR 33-46),中位数CD4 201细胞/ mm3(IQR 111-312),2年累积死亡率从1.9%(95%CI 1.7%)增加-2.0%)到7.0%(95%CI 5.7%-8.4%)(所有ART用户)的校正率,以及从2.1%(95%CI 1.8%-2.4%)到8.3%(95%CI 6.1%- 10.7%)(新的抗病毒药物使用者)修订后的省死亡率是新抗病毒药物使用者天真的死亡率的3-9倍,在卢萨卡省最低(每100人年4.6),在西部省份最高(8。更正后,每100人年7个)。校正后的死亡率因诊所而异,即使调整了临床(例如,治疗前的CD4)和环境,在新的ART使用者中,IQR为每100人年3.5至7.5例死亡,也高达每100人年13.4例死亡(例如,省和诊所规模)因素。死亡率(所有抗病毒治疗使用者)在治疗后的第一年最高,分别为4.6 / 100人年(95%CI 3.9-5.5),第二年2.9 / 100人年(95%CI 2.1-3.9)和大约1.6每年8%的治疗年限。在多变量分析中,包括男性,治疗前CD4水平和WHO分期在内的患者水平因素与新ART使用者的死亡率较高相关,而男性和HIV暴露与所有ART使用者的死亡率相关。在这两种情况下,都迟到(> 与死亡相关的时间为迟到14天)或丢失(迟到的时间超过90天)。我们无法确定约有四分之一丢失和被选中进行追踪的人的生命状况,也没有确定死亡原因。结论赞比亚的艾滋病毒治疗并非最佳效果。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。我们无法确定约有四分之一丢失和被选中进行追踪的人的生命状况,也没有确定死亡原因。结论赞比亚的艾滋病毒治疗并非最佳效果。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。我们无法确定约有四分之一丢失和被选中进行追踪的人的生命状况,也没有确定死亡原因。结论赞比亚的艾滋病毒治疗并非最佳效果。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。
更新日期:2018-02-01
中文翻译:

在赞比亚4个省中,活跃患者和失去随访的患者中HIV治疗的估计死亡率:基于多阶段抽样调查的结果。
背景技术存活率是成功治疗HIV的最重要的单一指标。例行监测未能捕获大多数死亡。结果,对艾滋病毒服务影响的区域评估和为改进工作而确定的热点都受到限制。我们试图评估治疗中的真实死亡率,表征赞比亚常规卫生信息系统中死亡率低报的程度,并使用多阶段,地区代表性的抽样方法确定各地间和一段时间内的死亡率驱动因素。方法和研究结果我们列举了所有接受抗逆转录病毒疗法(ART)感染HIV的成年人,他们在2013年8月1日至2015年7月31日的24个月内访问了赞比亚4个省的64个设施中的任何一个。通过选择与规模成正比的设施概率,然后选择一个简单的随机丢失患者样本,我们确定了丢失随访患者的概率样本。失去随访的患者的结果通过概率加权纳入生存分析和多元回归。在165,464个人中(64%女性,中位年龄39岁(IQR 33-46),中位数CD4 201细胞/ mm3(IQR 111-312),2年累积死亡率从1.9%(95%CI 1.7%)增加-2.0%)到7.0%(95%CI 5.7%-8.4%)(所有ART用户)的校正率,以及从2.1%(95%CI 1.8%-2.4%)到8.3%(95%CI 6.1%- 10.7%)(新的抗病毒药物使用者)修订后的省死亡率是新抗病毒药物使用者天真的死亡率的3-9倍,在卢萨卡省最低(每100人年4.6),在西部省份最高(8。更正后,每100人年7个)。校正后的死亡率因诊所而异,即使调整了临床(例如,治疗前的CD4)和环境,在新的ART使用者中,IQR为每100人年3.5至7.5例死亡,也高达每100人年13.4例死亡(例如,省和诊所规模)因素。死亡率(所有抗病毒治疗使用者)在治疗后的第一年最高,分别为4.6 / 100人年(95%CI 3.9-5.5),第二年2.9 / 100人年(95%CI 2.1-3.9)和大约1.6每年8%的治疗年限。在多变量分析中,包括男性,治疗前CD4水平和WHO分期在内的患者水平因素与新ART使用者的死亡率较高相关,而男性和HIV暴露与所有ART使用者的死亡率相关。在这两种情况下,都迟到(> 与死亡相关的时间为迟到14天)或丢失(迟到的时间超过90天)。我们无法确定约有四分之一丢失和被选中进行追踪的人的生命状况,也没有确定死亡原因。结论赞比亚的艾滋病毒治疗并非最佳效果。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。我们无法确定约有四分之一丢失和被选中进行追踪的人的生命状况,也没有确定死亡原因。结论赞比亚的艾滋病毒治疗并非最佳效果。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。我们无法确定约有四分之一丢失和被选中进行追踪的人的生命状况,也没有确定死亡原因。结论赞比亚的艾滋病毒治疗并非最佳效果。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。较高的持续死亡率和在省一级的死亡率报告不足以及区域和地点之间无法解释的异质性表明,有机会使用校正后的死亡率来改善质量。区域代表性的基于抽样的方法可以使计划的差距和机会成为地方和全球决策者明确的流行病学重点。











































 京公网安备 11010802027423号
京公网安备 11010802027423号