JAMA Oncology ( IF 22.5 ) Pub Date : 2018-01-01 , DOI: 10.1001/jamaoncol.2017.1879 Hiten D Patel 1, 2 , Jeffrey J Tosoian 1, 2 , H Ballentine Carter 1, 2 , Jonathan I Epstein 1, 2, 3
|
Importance Active surveillance is recommended for patients with very low-risk (VLR) and low-risk (LR) prostate cancer. Despite controversy, recent clinical guidelines state surveillance may be considered for men with low-volume intermediate-risk (LVIR) disease.
Objective To compare rates of adverse pathologic findings among VLR, LR, and LVIR men electing immediate radical prostatectomy and evaluate criteria to define if a favorable intermediate-risk group minimizing risk exists.
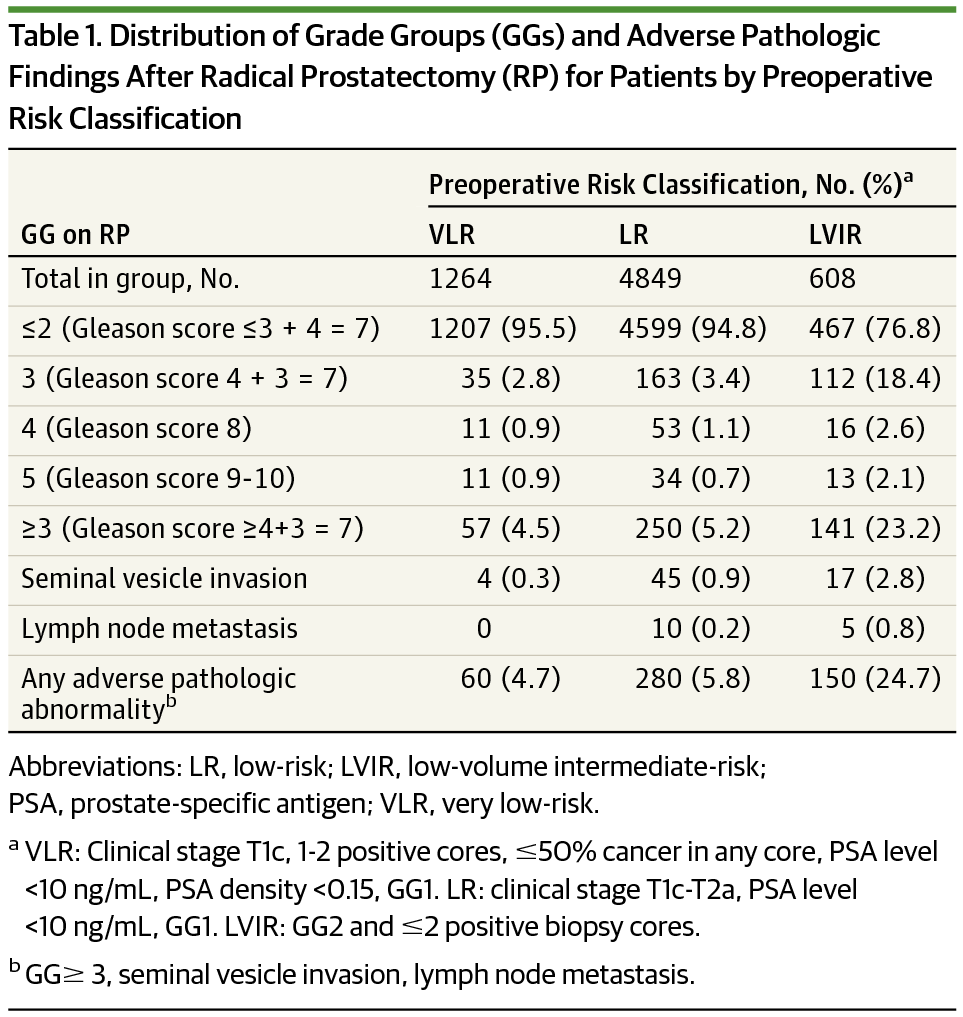
Design, Setting, and Participants This was a cohort study of men (2005-July 2016) with clinically localized VLR (1264 patients), LR (4849 patients), and LVIR (608 patients) (1-2 cores, Gleason 3 + 4 = 7, prostate-specific antigen [PSA] level <20 ng/mL) prostate cancer undergoing radical prostatectomy evaluated retrospectively at Johns Hopkins Hospital.
Interventions Radical prostatectomy.
Main Outcomes and Measures The proportions of men found to have at least Gleason 4 + 3 = 7 disease and other adverse pathologic features were compared by risk group. Log-binomial regression calculated relative risk (RR) of adverse pathologic findings in the LVIR cohort compared with VLR and LR cohorts. Analyses were repeated in subgroups of the LVIR population who otherwise met criteria for VLR (T1c, PSA density [PSAD] <0.15 ng/mL/cm3, ≤50% cancer in any core) and LR (≤T2a, PSA level <10 ng/mL) disease. Rates of adverse pathologic findings within the LVIR group were calculated based on various clinical thresholds, and univariable and multivariable logistic regression analyses were performed to identify predictors of adverse pathologic findings.
Results The rate of adverse pathologic findings was significantly higher for LVIR disease (150 of 608 patients [24.7%]; RR, 4.50; 95% CI, 3.73-5.43; P < .001) compared with LR disease (280 of 4849 [5.8%]), and LVIR disease (RR, 5.14; 95% CI, 3.84-6.89; P < .001) compared with men with VLR disease (60 of 1264 [4.7%]). Restriction of LVIR men to additional criteria did not significantly affect results. There were no preoperative clinical or pathologic criteria that could identify a subgroup of the LVIR population with rates of adverse pathologic findings comparable with those of the VLR and LR cohorts. PSAD was a significant predictor of adverse pathologic findings, but Gleason score had the largest effect (odds ratio, 4.30 (95% CI, 3.40-5.44; P < .001).
Conclusions and Relevance Nearly 25% of men (150 of 608) electing immediate radical prostatectomy with low-volume, Gleason 3 + 4 prostate cancer on biopsy are found to harbor adverse surgical pathologic findings. These data do not support the presence of a “favorable” subgroup among included patients and could have important implications for active surveillance in similar patients with Gleason 3 + 4 = 7 prostate cancer.
中文翻译:

男性选择即刻根治性前列腺切除术的不良病理结果定义有利的中度风险组
重要性 建议对极低风险 (VLR) 和低风险 (LR) 前列腺癌患者进行主动监测。尽管存在争议,但最近的临床指南状态监测可考虑用于患有低容量中危 (LVIR) 疾病的男性。
目的 比较选择即刻根治性前列腺切除术的 VLR、LR 和 LVIR 男性的不良病理结果发生率,并评估标准以确定是否存在将风险最小化的有利中危组。
设计、设置和参与者 这是一项针对男性(2005 年至 2016 年 7 月)进行的队列研究,其中包括临床局限性 VLR(1264 名患者)、LR(4849 名患者)和 LVIR(608 名患者)(1-2 个核心,Gleason 3 + 4 = 7,前列腺特异性抗原 [PSA] 水平 <20 ng/mL) 在约翰霍普金斯医院对接受根治性前列腺切除术的前列腺癌进行了回顾性评估。
干预 根治性前列腺切除术。
主要结果和措施 按风险组比较发现至少患有 Gleason 4 + 3 = 7 疾病和其他不良病理特征的男性比例。与 VLR 和 LR 队列相比,对数二项式回归计算了 LVIR 队列中不良病理结果的相对风险 (RR)。在符合 VLR(T1c,PSA 密度 [PSAD] <0.15 ng/mL/cm 3,任何核心≤50% 癌症)和 LR(≤T2a,PSA 水平 <10)标准的 LVIR 人群亚组中重复分析ng/mL) 疾病。根据各种临床阈值计算 LVIR 组内不良病理结果的发生率,并进行单变量和多变量逻辑回归分析以确定不良病理结果的预测因子。
结果 与 LR 疾病(4849 例患者中的 280 例[ 5.8 %])和 LVIR 疾病(RR,5.14;95% CI,3.84-6.89;P < .001)与患有 VLR 疾病的男性(1264 名中的 60 名 [4.7%])进行比较。将 LVIR 男性限制在其他标准并没有显着影响结果。没有术前临床或病理标准可以识别出 LVIR 人群的亚组,其不良病理发现率与 VLR 和 LR 组相当。PSAD 是不良病理结果的显着预测因子,但 Gleason 评分的影响最大(优势比,4.30(95% CI,3.40-5.44;P < .001)。
结论和相关性 近 25% 的男性(608 人中的 150 人)选择立即根治性前列腺切除术和小体积、Gleason 3 + 4 前列腺癌活检发现有不良的手术病理结果。这些数据不支持在纳入的患者中存在“有利的”亚组,并且可能对类似的格里森 3 + 4 = 7 前列腺癌患者的主动监测具有重要意义。











































 京公网安备 11010802027423号
京公网安备 11010802027423号