JAMA Oncology ( IF 22.5 ) Pub Date : 2018-08-01 , DOI: 10.1001/jamaoncol.2017.4504 Todd A. Pezzi 1 , David L. Schwartz 1, 2 , Abdallah S. R. Mohamed 1, 3 , James W. Welsh 1 , Ritsuko U. Komaki 1 , Stephen M. Hahn 1 , Boris Sepesi 4 , Christopher M. Pezzi 5 , Clifton D. Fuller 1 , Stephen G. Chun 1
|
Importance Combined-modality therapy with chemotherapy and radiation therapy plays a crucial role in the upfront treatment of patients with limited-stage small cell lung cancer (SCLC), but there may be barriers to utilization in the United States.
Objective To estimate utilization rates and factors associated with chemotherapy and radiation therapy delivery for limited-stage SCLC using the National Cancer Database.
Design, Setting, and Participants Analysis of initial management of all limited-stage SCLC cases from 2004 through 2013 in the National Cancer Database.
Main Outcomes and Measures Utilization rates of chemotherapy and radiation therapy at time of initial treatment. Multivariable analysis identified independent clinical and socioeconomic factors associated with utilization and overall survival.
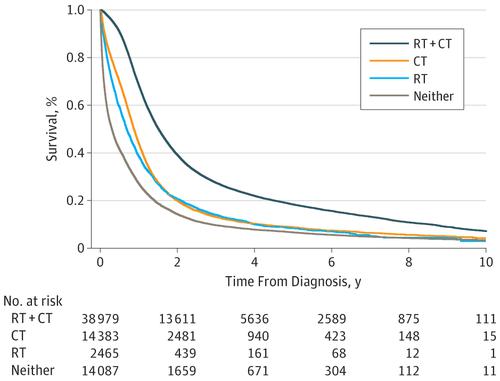
Results A total of 70 247 cases met inclusion criteria (55.3% female; median age, 68 y [range, 19-90 y]). Initial treatment was 55.5% chemotherapy and radiation therapy, 20.5% chemotherapy alone, 3.5% radiation therapy alone, and 20.0% neither (0.5% not reported). Median survival was 18.2 (95% CI, 17.9-18.4), 10.5 (95% CI, 10.3-10.7), 8.3 (95% CI, 7.7-8.8), and 3.7 (95% CI, 3.5-3.8) months, respectively. Being uninsured was associated with a lower likelihood of both chemotherapy (odds ratio [OR], 0.65; 95% CI, 0.56-0.75; P < .001) and radiation therapy (OR, 0.75; 95% CI, 0.67-0.85; P < .001) administration on multivariable analysis. Medicare/Medicaid insurance had no impact on chemotherapy use, whereas Medicaid (OR, 0.79; 95% CI, 0.72-0.87; P < .001) and Medicare (OR, 0.86; 95% CI, 0.82-0.91; P < .001) were independently associated with a lower likelihood of radiation therapy delivery. Lack of health insurance (HR, 1.19; 95% CI, 1.13-1.26; P < .001), Medicaid (HR, 1.27; 95% CI, 1.21-1.32; P < .001), and Medicare (HR, 1.12; 95% CI, 1.09-1.15; P < .001) coverage were independently associated with shorter survival on adjusted analysis, while chemotherapy (HR, 0.55; 95% CI, 0.54-0.57; P < .001) and radiation therapy (HR, 0.62; 95% CI, 0.60-0.63; P < .001) were associated with a survival benefit.
Conclusions and Relevance Substantial proportions of patients documented in a major US cancer registry did not receive radiation therapy or chemotherapy as part of initial treatment for limited-stage SCLC, which, in turn, was associated with poor survival. Lack of radiation therapy delivery was uniquely associated with government insurance coverage, suggesting a need for targeted access improvement in this population. Additional work will be necessary to conclusively define exact population patterns, specific treatment deficiencies, and causative factors leading to heterogeneous care delivery.
中文翻译:

限期小细胞肺癌联合治疗的障碍
重要性 联合疗法联合化学疗法和放射疗法在有限期小细胞肺癌(SCLC)患者的前期治疗中起着至关重要的作用,但在美国可能存在使用障碍。
目的 使用国家癌症数据库评估有限期SCLC的化学疗法和放射疗法的使用率和相关因素。
国家癌症数据库中2004年至2013年期间所有有限期SCLC病例的初始治疗的设计,背景和参与者分析。
主要结果和措施 初始治疗时化学疗法和放射疗法的利用率。多变量分析确定了与利用率和总体生存率相关的独立临床和社会经济因素。
结果 共有70 247例患者符合纳入标准(女性55.3%;中位年龄68岁[范围:19-90岁])。初始治疗为55.5%的化学疗法和放射疗法,单独的20.5%的化学疗法,单独的3.5%的放射疗法,以及20.0%的都不是(未报道0.5%)。中位生存期分别为18.2(95%CI,17.9-18.4),10.5(95%CI,10.3-10.7),8.3(95%CI,7.7-8.8)和3.7(95%CI,3.5-3.8)月。 。未投保与较低的化学疗法(优势比[OR],0.65; 95%CI,0.56-0.75;P <.001)和放射疗法(OR,0.75; 95%CI,0.67-0.85;P <.001)进行多变量分析。Medicare / Medicaid保险对化疗的使用没有影响,而Medicaid(OR为0.79; 95%CI为0.72-0.87;P <.001)和Medicare(OR,0.86; 95%CI,0.82-0.91; P <.001)与较低的放射治疗可能性独立相关。缺乏健康保险(HR,1.19; 95%CI,1.13-1.26; P <.001),Medicaid(HR,1.27; 95%CI,1.21-1.32; P <.001)和Medicare(HR,1.12; 经校正后的分析表明,95%CI(1.09-1.15; P <.001)的覆盖率与生存期的缩短独立相关,而化学疗法(HR,0.55; 95%CI,0.54-0.57; P <.001)和放射疗法(HR, 0.62; 95%CI,0.60-0.63; P <.001)与生存获益相关。
结论和相关性 在美国主要癌症登记处记录的大量患者没有接受放射治疗或化学疗法作为有限期SCLC初始治疗的一部分,这反过来又与生存期差有关。缺乏放射治疗与政府保险的覆盖率有独特的联系,这表明需要有针对性地改善这一人群。为了确定确切的人群模式,特定的治疗缺陷以及导致提供异质医疗的原因,将需要进行额外的工作。











































 京公网安备 11010802027423号
京公网安备 11010802027423号