JAMA Surgery ( IF 15.7 ) Pub Date : 2018-05-01 , DOI: 10.1001/jamasurg.2017.5150 Russell J. Funk 1 , Jason Owen-Smith 2 , Samuel A. Kaufman 3 , Brahmajee K. Nallamothu 4, 5 , John M. Hollingsworth 3
|
Importance To reduce inefficiency and waste associated with care fragmentation, many current programs target greater clinical integration among physicians. However, these programs have led to only modest Medicare spending reductions. Most programs focus on formal integration, which often bears little resemblance to actual physician interaction patterns.
Objectives To examine how physician interaction patterns vary between health systems and to assess whether variation in informal integration is associated with care delivery payments.
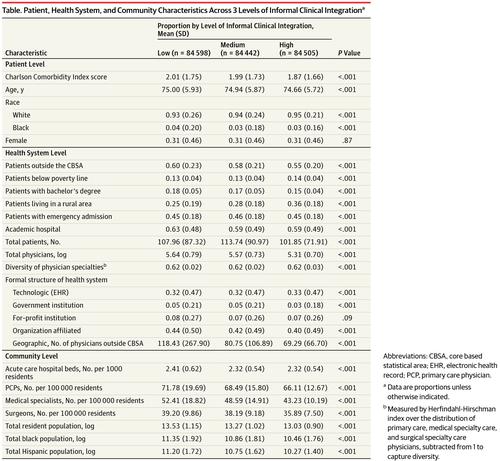
Design, Setting, and Participants National Medicare data from January 1, 2008, through December 31, 2011, identified 253 545 Medicare beneficiaries (aged ≥66 years) from 1186 health systems where Medicare beneficiaries underwent coronary artery bypass grafting (CABG) procedures. Interactions were mapped between all physicians who treated these patients—including primary care physicians and surgical and medical specialists—within a health system during their surgical episode. The level of informal integration was measured in these networks of interacting physicians. Multivariate regression models were fitted to evaluate associations between payments for each surgical episode made on a beneficiary’s behalf and the level of informal integration in the health system where the patient was treated.
Exposures The informal integration level of a health system.
Main Outcomes and Measures Price-standardized total surgical episode and component payments.
Results The total 253 545 study participants included 175 520 men (69.2%; mean [SD] age, 74.51 [5.75] years) and 78 024 women (34.3%; 75.67 [5.91] years). One beneficiary of the 253 545 participants did not have sex information. The low level of informal clinical integration included 84 598 patients (33.4%; mean [SD] age, 75.00 [5.93] years); medium level, 84 442 (33.30%; 74.94 [5.87] years); and high level, 84 505 (33.34%; 74.66 [5.72] years) (P < .001). Informal integration levels varied across health systems. After adjusting for patient, health-system, and community factors, higher levels of informal integration were associated with significantly lower total episode and component payments (β coefficients for informal integration were −365.87 [95% CI, −451.08 to −280.67] for total episode payments, −182.63 [−239.80 to −125.46] for index hospitalization, −43.13 [−55.53 to −30.72] for physician services, −74.48 [−103.45 to −45.51] for hospital readmissions, and −62.04 [−88.00 to −36.07] for postacute care; P < .001 for each association). When beneficiaries were treated in health systems with higher informal integration, the greatest savings of lower estimated payments were from hospital readmissions (13.0%) and postacute care services (5.8%).
Conclusions and Relevance Informal integration is associated with lower spending. Although most programs that seek to promote clinical integration are focused on health systems’ formal structures, policy makers may also want to address informal integration.
中文翻译:

医师非正式临床整合与心脏外科手术支付的关联
重要性 为了减少效率低下和与医疗服务分散相关的浪费,许多当前计划的目标是加强医师之间的临床整合。但是,这些计划仅导致适度的Medicare支出减少。大多数程序专注于形式整合,这通常与实际的医生互动模式几乎没有相似之处。
目的 研究卫生系统之间医生的互动模式如何变化,并评估非正式整合的变化是否与护理交付费用相关。
设计,设置和参与者 从2008年1月1日到2011年12月31日的国家医疗保险数据,从1186个医疗系统中进行了冠状动脉搭桥术(CABG)的1186个卫生系统中,确定了253 545名医疗保险受益者(年龄≥66岁)。在手术期间,在卫生系统内,在所有治疗这些患者的医生之间(包括初级保健医生以及外科和医学专家)之间的相互作用进行了映射。在这些互动的医生网络中测量了非正式整合的水平。拟合了多元回归模型,以评估代表受益人进行的每次外科手术的费用与治疗患者的医疗系统中非正式整合水平之间的关联。
暴露 卫生系统的非正式整合级别。
主要结果和措施 价格标准化的总手术发作和组成部分付款。
结果 总共253 545名研究参与者包括175 520名男性(69.2%;平均[SD]年龄,74.51 [5.75]岁)和78 024女性(34.3%; 75.67 [5.91]岁)。253 545名参与者中的一名受益人没有性别信息。非正式临床整合的低水平包括84 598名患者(33.4%;平均[SD]年龄为75.00 [5.93]岁);中级84 442(33.30%; 74.94 [5.87]年);高级别84 505(33.34%; 74.66 [5.72]年)(P <.001)。非正式整合水平在整个卫生系统中各不相同。在对患者,卫生系统和社区因素进行调整后,非正式融合的较高水平与总发作和组分支付的显着降低相关(非正式融合的β系数为-365.87 [95%CI,-451.08至-280.67]发作支付,指数住院的−182.63 [−239.80至−125.46],医师服务的−43.13 [−55.53至−30.72],住院再住院的−74.48 [−103.45至−45.51]和−62.04 [−88.00至- [36.07];用于急性后护理; 每个关联P <0.001)。当受益人在非正式一体化程度较高的卫生系统中得到治疗时,估计较低的付款最大的节省来自住院再入院(13.0%)和急诊后护理服务(5.8%)。
结论与相关性 非正式整合与较低的支出相关。尽管大多数旨在促进临床整合的计划都侧重于卫生系统的正式结构,但政策制定者也可能希望解决非正式整合问题。











































 京公网安备 11010802027423号
京公网安备 11010802027423号