Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Effect of Cervical Pessary on Spontaneous Preterm Birth in Women With Singleton Pregnancies and Short Cervical Length
JAMA ( IF 63.1 ) Pub Date : 2017-12-19 , DOI: 10.1001/jama.2017.18956 Gabriele Saccone 1 , Giuseppe Maria Maruotti 1 , Antonia Giudicepietro 1 , Pasquale Martinelli 1 ,
JAMA ( IF 63.1 ) Pub Date : 2017-12-19 , DOI: 10.1001/jama.2017.18956 Gabriele Saccone 1 , Giuseppe Maria Maruotti 1 , Antonia Giudicepietro 1 , Pasquale Martinelli 1 ,
Affiliation
|
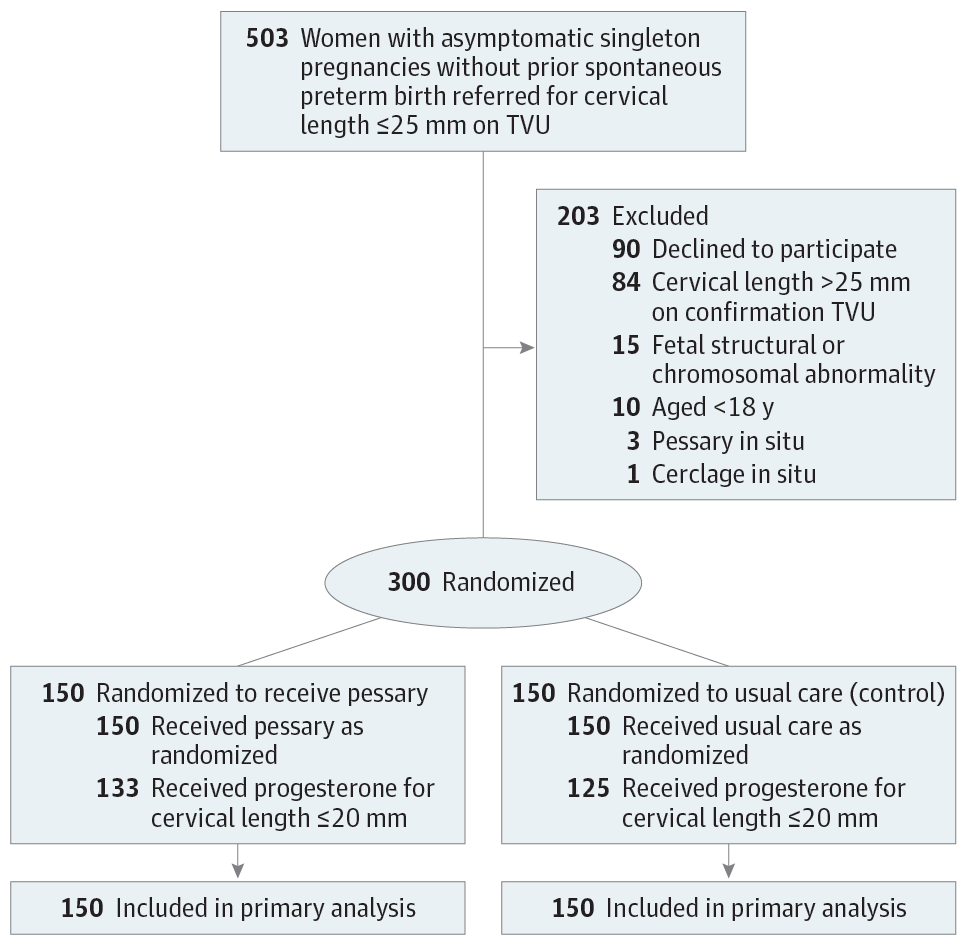
Importance Spontaneous preterm birth is a major cause of perinatal morbidity and mortality. It is unclear if a cervical pessary can reduce the risk of spontaneous preterm delivery. Objective To test whether in asymptomatic women with singleton pregnancies and no prior spontaneous preterm birth but with short cervical length on transvaginal ultrasound, use of a cervical pessary would reduce the rate of spontaneous preterm birth at less than 34 weeks of gestation. Design, Setting, and Participants Parallel-group, nonblinded, randomized clinical trial conducted from March 1, 2016, to May 25, 2017, at a single center in Italy. Asymptomatic women with singleton gestations, no previous spontaneous preterm births, and cervical lengths of 25 mm or less at 18 weeks 0 days to 23 weeks 6 days of gestation were eligible. Interventions Patients were randomized 1:1 to receive either cervical pessary (n = 150) or no pessary (n = 150). The pessary was removed between 37 weeks 0 days and 37 weeks 6 days of gestation or earlier if clinically indicated. The control group received standard care. For cervical length of 20 mm or shorter, women in both groups were prescribed vaginal progesterone, 200 mg/d, until 36 weeks 6 days of gestation. No bed rest or activity restriction was recommended. Main Outcomes and Measures The primary end point was spontaneous preterm birth at less than 34 weeks of gestation. Secondary outcomes were adverse events. Results Among 300 women who were randomized (mean age, 29 [SD, 6.3] years; mean gestational age, 22 [SD, 1.3] weeks), 100% completed the trial. The primary end point occurred in 11 women (7.3%) in the pessary group and 23 women (15.3%) in the control group (between-group difference, −8.0% [95% CI, −15.7% to −0.4]; relative risk, 0.48 [95% CI, 0.24-0.95]). During follow-up, the pessary group had a higher rate of increased or new vaginal discharge (86.7% vs 46.0%; between-group difference, +40.7% [95% CI, +30.1%-+50.3%]; relative risk, 1.88 [95% CI, 1.57-2.27]). Conclusions and Relevance Among women without prior spontaneous preterm birth who had asymptomatic singleton pregnancies and short transvaginal cervical length, use of a cervical pessary, compared with no pessary use, resulted in a lower rate of spontaneous preterm birth at less than 34 weeks of gestation. The results of this single-center, nonblinded study among selected pregnant women require confirmation in multicenter clinical trials. Trial Registration clinicaltrials.gov Identifier: NCT02716909
中文翻译:

宫颈托对宫颈过短单胎妊娠妇女自然早产的影响
重要性自然早产是围产期发病率和死亡率的主要原因。目前尚不清楚宫颈托是否可以降低自然早产的风险。目的 旨在测试无症状的单胎妊娠且既往无自发性早产但经阴道超声显示宫颈长度较短的女性,使用宫颈托是否会降低小于 34 周时自发性早产的发生率。设计、设置和参与者 平行组、非盲、随机临床试验于 2016 年 3 月 1 日至 2017 年 5 月 25 日在意大利的一个中心进行。无症状的单胎妊娠妇女、既往无自发性早产、妊娠第 18 周第 0 天至第 23 周第 6 天宫颈长度不超过 25 毫米的女性均符合条件。干预 患者按 1:1 随机接受宫颈托 (n = 150) 或不接受托 (n = 150)。如果有临床指征,在妊娠 37 周第 0 天和第 37 周第 6 天之间或更早时取出子宫托。对照组接受标准护理。对于宫颈长度为 20 毫米或更短的情况,两组女性均服用 200 毫克/天的阴道黄体酮,直至妊娠 36 周 6 天。不建议卧床休息或限制活动。主要结果和措施 主要终点是小于 34 周的自发早产。次要结果是不良事件。结果 在随机分组的 300 名妇女中(平均年龄,29 [SD,6.3] 岁;平均胎龄,22 [SD,1.3] 周),100% 完成了试验。主要终点发生在子宫托组的 11 名女性 (7.3%) 和 23 名女性 (15. 3%)在对照组(组间差异,-8.0% [95% CI,-15.7% 至 -0.4];相对风险,0.48 [95% CI,0.24-0.95])。在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 0% [95% CI,-15.7% 至 -0.4];相对风险,0.48 [95% CI,0.24-0.95])。在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 0% [95% CI,-15.7% 至 -0.4];相对风险,0.48 [95% CI,0.24-0.95])。在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 1%-+50.3%];相对风险,1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 1%-+50.3%];相对风险,1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 导致小于 34 周的自发早产率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 导致小于 34 周的自发早产率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909
更新日期:2017-12-19
中文翻译:

宫颈托对宫颈过短单胎妊娠妇女自然早产的影响
重要性自然早产是围产期发病率和死亡率的主要原因。目前尚不清楚宫颈托是否可以降低自然早产的风险。目的 旨在测试无症状的单胎妊娠且既往无自发性早产但经阴道超声显示宫颈长度较短的女性,使用宫颈托是否会降低小于 34 周时自发性早产的发生率。设计、设置和参与者 平行组、非盲、随机临床试验于 2016 年 3 月 1 日至 2017 年 5 月 25 日在意大利的一个中心进行。无症状的单胎妊娠妇女、既往无自发性早产、妊娠第 18 周第 0 天至第 23 周第 6 天宫颈长度不超过 25 毫米的女性均符合条件。干预 患者按 1:1 随机接受宫颈托 (n = 150) 或不接受托 (n = 150)。如果有临床指征,在妊娠 37 周第 0 天和第 37 周第 6 天之间或更早时取出子宫托。对照组接受标准护理。对于宫颈长度为 20 毫米或更短的情况,两组女性均服用 200 毫克/天的阴道黄体酮,直至妊娠 36 周 6 天。不建议卧床休息或限制活动。主要结果和措施 主要终点是小于 34 周的自发早产。次要结果是不良事件。结果 在随机分组的 300 名妇女中(平均年龄,29 [SD,6.3] 岁;平均胎龄,22 [SD,1.3] 周),100% 完成了试验。主要终点发生在子宫托组的 11 名女性 (7.3%) 和 23 名女性 (15. 3%)在对照组(组间差异,-8.0% [95% CI,-15.7% 至 -0.4];相对风险,0.48 [95% CI,0.24-0.95])。在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 0% [95% CI,-15.7% 至 -0.4];相对风险,0.48 [95% CI,0.24-0.95])。在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 0% [95% CI,-15.7% 至 -0.4];相对风险,0.48 [95% CI,0.24-0.95])。在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 在随访期间,子宫托组的阴道分泌物增加或新出现的比率更高(86.7% 对 46.0%;组间差异,+40.7% [95% CI,+30.1%-+50.3%];相对风险, 1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 1%-+50.3%];相对风险,1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 1%-+50.3%];相对风险,1.88 [95% CI,1.57-2.27])。结论和相关性 在没有既往无症状单胎妊娠且经阴道宫颈长度较短的女性中,使用宫颈托与未使用宫颈托相比,在妊娠 34 周内发生自发性早产的几率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 导致小于 34 周的自发早产率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909 导致小于 34 周的自发早产率较低。这项在选定孕妇中进行的单中心非盲研究的结果需要多中心临床试验的确认。试验注册clinicaltrials.gov 标识符:NCT02716909









































 京公网安备 11010802027423号
京公网安备 11010802027423号