当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Effect of Technique on Outcomes Following Bioresorbable Vascular Scaffold Implantation
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2017-12-01 , DOI: 10.1016/j.jacc.2017.09.1106 Gregg W Stone 1 , Alexandre Abizaid 2 , Yoshinobu Onuma 3 , Ashok Seth 4 , Runlin Gao 5 , John Ormiston 6 , Takeshi Kimura 7 , Bernard Chevalier 8 , Ori Ben-Yehuda 1 , Ovidiu Dressler 9 , Tom McAndrew 9 , Stephen G Ellis 10 , Dean J Kereiakes 11 , Patrick W Serruys 12
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2017-12-01 , DOI: 10.1016/j.jacc.2017.09.1106 Gregg W Stone 1 , Alexandre Abizaid 2 , Yoshinobu Onuma 3 , Ashok Seth 4 , Runlin Gao 5 , John Ormiston 6 , Takeshi Kimura 7 , Bernard Chevalier 8 , Ori Ben-Yehuda 1 , Ovidiu Dressler 9 , Tom McAndrew 9 , Stephen G Ellis 10 , Dean J Kereiakes 11 , Patrick W Serruys 12
Affiliation
|
BACKGROUND
Procedural technique may affect clinical outcomes after bioresorbable vascular scaffold (BVS) implantation. Prior studies suggesting such a relationship have not adjusted for baseline patient and lesion characteristics that may have influenced operator choice of technique and outcomes. OBJECTIVES
This study sought to determine whether target lesion failure (TLF) (cardiac death, target-vessel myocardial infarction, or ischemia-driven target lesion revascularization) and scaffold thrombosis (ScT) rates within 3 years of BVS implantation are affected by operator technique (vessel size selection and pre- and post-dilation parameters). METHODS
TLF and ScT rates were determined in 2,973 patients with 3,149 BVS-treated coronary artery lesions from 5 prospective studies (ABSORB II, ABSORB China, ABSORB Japan, ABSORB III, and ABSORB Extend). Outcomes through 3 years (and between 0 to 1 and 1 to 3 years) were assessed according to pre-specified definitions of optimal technique (pre-dilation, vessel sizing, and post-dilation). Multivariable analysis was used to adjust for differences in up to 18 patient and lesion characteristics. RESULTS
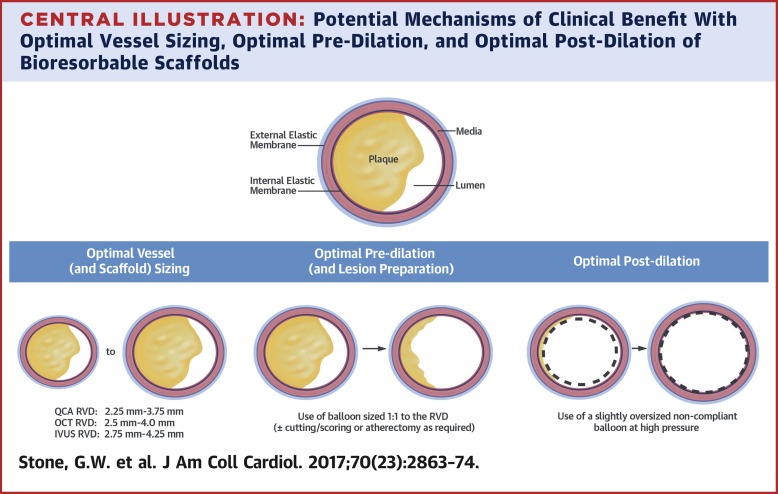
Optimal pre-dilation (balloon to core laboratory-derived reference vessel diameter ratio ≥1:1), vessel size selection (reference vessel diameter ≥2.25 mm and ≤3.75 mm), and post-dilation (with a noncompliant balloon at ≥18 atm and larger than the nominal scaffold diameter, but not by >0.5 mm larger) in all BVS-treated lesions were performed in 59.2%, 81.6%, and 12.4% of patients, respectively. BVS implantation in properly sized vessels was an independent predictor of freedom from TLF through 1 year (hazard ratio [HR]: 0.67; p = 0.01) and through 3 years (HR: 0.72; p = 0.01), and of freedom from ScT through 1 year (HR: 0.36; p = 0.004). Aggressive pre-dilation was an independent predictor of freedom from ScT between 1 and 3 years (HR: 0.44; p = 0.03), and optimal post-dilation was an independent predictor of freedom from TLF between 1 and 3 years (HR: 0.55; p = 0.05). CONCLUSIONS
In the present large-scale analysis from the major ABSORB studies, after multivariable adjustment for baseline patient and lesion characteristics, vessel sizing and operator technique were strongly associated with BVS-related outcomes during 3-year follow-up. (ABSORB II Randomized Controlled Trial [ABSORB II]; NCT01425281; ABSORB III Randomized Controlled Trial [RCT] [ABSORB-III]; NCT01751906; A Clinical Evaluation of Absorb Bioresorbable Vascular Scaffold [Absorb BVS] System in Chinese Population-ABSORB CHINA Randomized Controlled Trial [RCT] [ABSORB CHINA]; NCT01923740; ABSORB EXTEND Clinical Investigation [ABSORB EXTEND]; NCT01023789; AVJ-301 Clinical Trial: A Clinical Evaluation of AVJ-301 [Absorb BVS] in Japanese Population [ABSORB JAPAN]; NCT01844284).
更新日期:2017-12-01











































 京公网安备 11010802027423号
京公网安备 11010802027423号