Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association Between Treatment by Locum Tenens Internal Medicine Physicians and 30-Day Mortality Among Hospitalized Medicare Beneficiaries
JAMA ( IF 63.1 ) Pub Date : 2017-12-05 , DOI: 10.1001/jama.2017.17925 Daniel M. Blumenthal 1 , Andrew R. Olenski 2 , Yusuke Tsugawa 3 , Anupam B. Jena 4
JAMA ( IF 63.1 ) Pub Date : 2017-12-05 , DOI: 10.1001/jama.2017.17925 Daniel M. Blumenthal 1 , Andrew R. Olenski 2 , Yusuke Tsugawa 3 , Anupam B. Jena 4
Affiliation
|
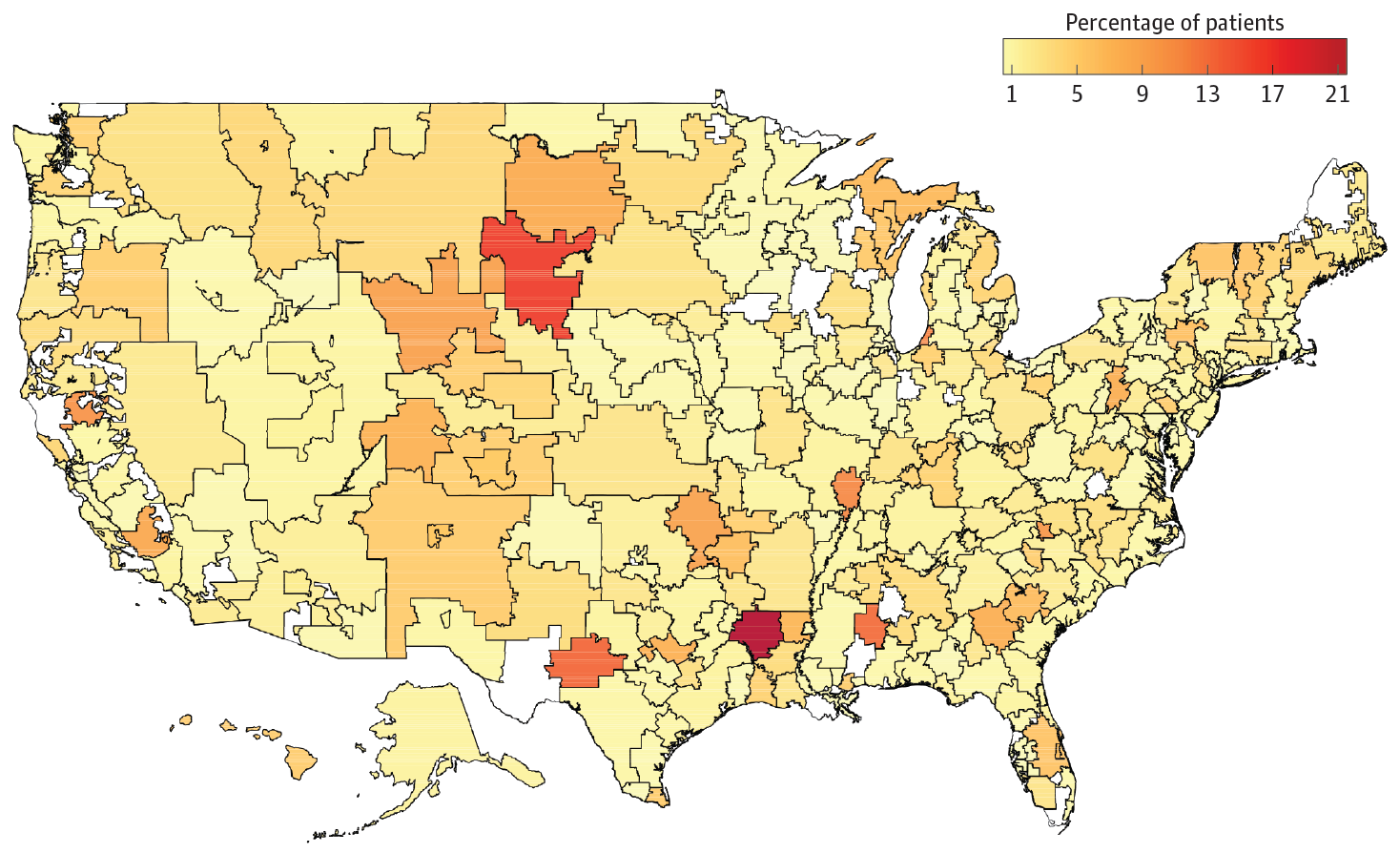
Importance Use of locum tenens physicians has increased in the United States, but information about their quality and costs of care is lacking. Objective To evaluate quality and costs of care among hospitalized Medicare beneficiaries treated by locum tenens vs non–locum tenens physicians. Design, Setting, and Participants A random sample of Medicare fee-for-service beneficiaries hospitalized during 2009-2014 was used to compare quality and costs of hospital care delivered by locum tenens and non–locum tenens internal medicine physicians. Exposures Treatment by locum tenens general internal medicine physicians. Main Outcomes and Measures The primary outcome was 30-day mortality. Secondary outcomes included inpatient Medicare Part B spending, length of stay, and 30-day readmissions. Differences between locum tenens and non–locum tenens physicians were estimated using multivariable logistic regression models adjusted for beneficiary clinical and demographic characteristics and hospital fixed effects, which enabled comparisons of clinical outcomes between physicians practicing within the same hospital. In prespecified subgroup analyses, outcomes were reevaluated among hospitals with different levels of intensity of locum tenens physician use. Results Of 1 818 873 Medicare admissions treated by general internists, 38 475 (2.1%) received care from a locum tenens physician; 9.3% (4123/44 520) of general internists were temporarily covered by a locum tenens physician at some point. Differences in patient characteristics, demographics, comorbidities, and reason for admission between locum tenens and non–locum tenens physicians were not clinically relevant. Treatment by locum tenens physicians, compared with treatment by non–locum tenens physicians (n = 44 520 physicians), was not associated with a significant difference in 30-day mortality (8.83% vs 8.70%; adjusted difference, 0.14%; 95% CI, −0.18% to 0.45%). Patients treated by locum tenens physicians had significantly higher Part B spending ($1836 vs $1712; adjusted difference, $124; 95% CI, $93 to $154), significantly longer mean length of stay (5.64 days vs 5.21 days; adjusted difference, 0.43 days; 95% CI, 0.34 to 0.52), and significantly lower 30-day readmissions (22.80% vs 23.83%; adjusted difference, −1.00%; 95% CI −1.57% to −0.54%). Conclusions and Relevance Among hospitalized Medicare beneficiaries treated by a general internist, there were no significant differences in overall 30-day mortality rates among patients treated by locum tenens compared with non–locum tenens physicians. Additional research may help determine hospital-level factors associated with the quality and costs of care related to locum tenens physicians.
中文翻译:

Locum Tenens内科医师治疗与住院医疗保险受益人30天死亡率的关系
重要性 在美国,当地医生的使用有所增加,但缺乏关于他们的质量和护理成本的信息。目的 评估由临时工与非临时工医生治疗的住院医疗保险受益人的护理质量和成本。设计、设置和参与者 使用 2009-2014 年住院的医疗保险按服务付费受益人的随机样本来比较临时和非临时内科医师提供的医院护理的质量和成本。暴露治疗由 locum tenens 一般内科医师进行。主要结果和措施 主要结果是 30 天死亡率。次要结果包括住院医疗保险 B 部分支出、住院时间和 30 天再入院。使用根据受益人的临床和人口统计学特征以及医院固定效应调整的多变量逻辑回归模型估计了专职医生和非专职医生之间的差异,从而能够比较同一医院内执业医生之间的临床结果。在预先指定的亚组分析中,对不同程度的医生使用强度水平的医院的结果进行了重新评估。结果 在由普通内科医生治疗的 1 818 873 名 Medicare 入院患者中,38 475 人(2.1%)接受了专科医师的护理;9.3% (4123/44 520) 的普通内科医生在某个时候被临时内科医生覆盖。患者特征、人口统计学、合并症、中医和非中医医师之间的入院原因与临床无关。与非执业医师(n = 44 520 名医师)的治疗相比,由专职医师进行的治疗与 30 天死亡率的显着差异无关(8.83% 对 8.70%;调整后的差异,0.14%;95%) CI,-0.18% 至 0.45%)。由 locum tenens 医生治疗的患者的 B 部分支出明显更高(1836 美元与 1712 美元;调整后差异,124 美元;95% CI,93 至 154 美元),平均住院时间明显更长(5.64 天与 5.21 天;调整后差异,0.43 天; 95% CI,0.34 至 0.52),30 天再入院率显着降低(22.80% 对 23.83%;调整后差异,-1.00%;95% CI -1.57% 至 -0.54%)。结论和相关性在由普通内科医生治疗的住院医疗保险受益人中,与非 Locum tenens 医生相比,使用 Locum tenens 治疗的患者的 30 天总死亡率没有显着差异。其他研究可能有助于确定与当地医生相关的护理质量和成本相关的医院级因素。
更新日期:2017-12-05
中文翻译:

Locum Tenens内科医师治疗与住院医疗保险受益人30天死亡率的关系
重要性 在美国,当地医生的使用有所增加,但缺乏关于他们的质量和护理成本的信息。目的 评估由临时工与非临时工医生治疗的住院医疗保险受益人的护理质量和成本。设计、设置和参与者 使用 2009-2014 年住院的医疗保险按服务付费受益人的随机样本来比较临时和非临时内科医师提供的医院护理的质量和成本。暴露治疗由 locum tenens 一般内科医师进行。主要结果和措施 主要结果是 30 天死亡率。次要结果包括住院医疗保险 B 部分支出、住院时间和 30 天再入院。使用根据受益人的临床和人口统计学特征以及医院固定效应调整的多变量逻辑回归模型估计了专职医生和非专职医生之间的差异,从而能够比较同一医院内执业医生之间的临床结果。在预先指定的亚组分析中,对不同程度的医生使用强度水平的医院的结果进行了重新评估。结果 在由普通内科医生治疗的 1 818 873 名 Medicare 入院患者中,38 475 人(2.1%)接受了专科医师的护理;9.3% (4123/44 520) 的普通内科医生在某个时候被临时内科医生覆盖。患者特征、人口统计学、合并症、中医和非中医医师之间的入院原因与临床无关。与非执业医师(n = 44 520 名医师)的治疗相比,由专职医师进行的治疗与 30 天死亡率的显着差异无关(8.83% 对 8.70%;调整后的差异,0.14%;95%) CI,-0.18% 至 0.45%)。由 locum tenens 医生治疗的患者的 B 部分支出明显更高(1836 美元与 1712 美元;调整后差异,124 美元;95% CI,93 至 154 美元),平均住院时间明显更长(5.64 天与 5.21 天;调整后差异,0.43 天; 95% CI,0.34 至 0.52),30 天再入院率显着降低(22.80% 对 23.83%;调整后差异,-1.00%;95% CI -1.57% 至 -0.54%)。结论和相关性在由普通内科医生治疗的住院医疗保险受益人中,与非 Locum tenens 医生相比,使用 Locum tenens 治疗的患者的 30 天总死亡率没有显着差异。其他研究可能有助于确定与当地医生相关的护理质量和成本相关的医院级因素。











































 京公网安备 11010802027423号
京公网安备 11010802027423号