当前位置:
X-MOL 学术
›
JAMA Pediatr.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Neurodevelopmental and Behavioral Outcomes in Extremely Premature Neonates With Ventriculomegaly in the Absence of Periventricular-Intraventricular Hemorrhage
JAMA Pediatrics ( IF 26.1 ) Pub Date : 2018-01-01 , DOI: 10.1001/jamapediatrics.2017.3545 Athina Pappas 1 , Ira Adams-Chapman 2 , Seetha Shankaran 1 , Scott A. McDonald 3 , Barbara J. Stoll 4 , Abbot R. Laptook 5 , Waldemar A. Carlo 6 , Krisa P. Van Meurs 7 , Susan R. Hintz 7 , Martha D. Carlson 8 , Jane E. Brumbaugh 9, 10 , Michele C. Walsh 11 , Myra H. Wyckoff 12 , Abhik Das 13 , Rosemary D. Higgins 14 ,
JAMA Pediatrics ( IF 26.1 ) Pub Date : 2018-01-01 , DOI: 10.1001/jamapediatrics.2017.3545 Athina Pappas 1 , Ira Adams-Chapman 2 , Seetha Shankaran 1 , Scott A. McDonald 3 , Barbara J. Stoll 4 , Abbot R. Laptook 5 , Waldemar A. Carlo 6 , Krisa P. Van Meurs 7 , Susan R. Hintz 7 , Martha D. Carlson 8 , Jane E. Brumbaugh 9, 10 , Michele C. Walsh 11 , Myra H. Wyckoff 12 , Abhik Das 13 , Rosemary D. Higgins 14 ,
Affiliation
|
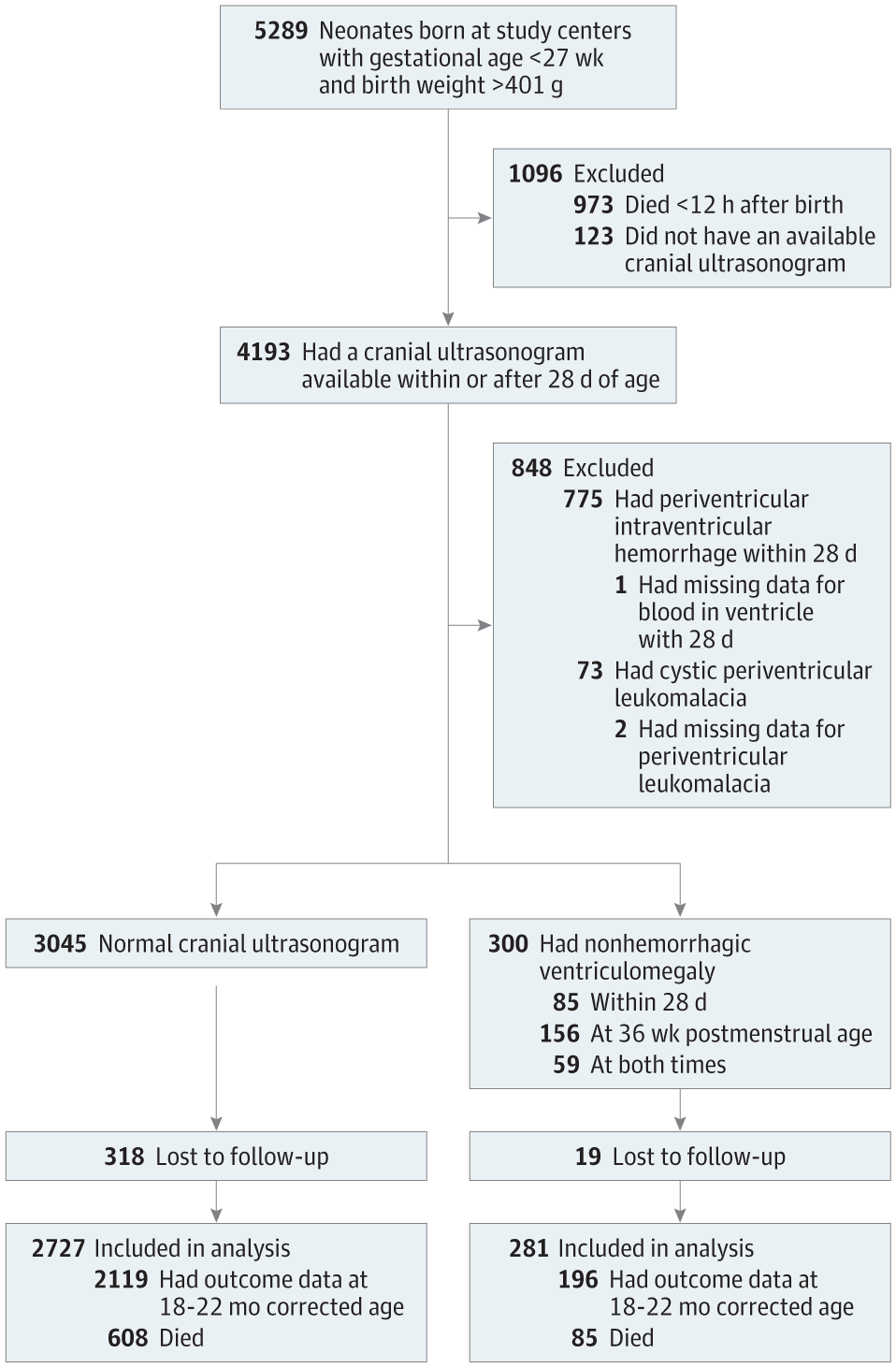
Importance Studies of cranial ultrasonography and early childhood outcomes among cohorts of extremely preterm neonates have linked periventricular-intraventricular hemorrhage and cystic periventricular leukomalacia with adverse neurodevelopmental outcomes. However, the association between nonhemorrhagic ventriculomegaly and neurodevelopmental and behavioral outcomes is not fully understood. Objective To characterize the outcomes of extremely preterm neonates younger than 27 weeks’ gestational age who experienced nonhemorrhagic ventriculomegaly that was detected prior to 36 weeks’ postmenstrual age. Design, Setting, and Participants This longitudinal observational study was conducted at 16 centers of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Infants born prior to 27 weeks’ gestational age in any network facility between July 1, 2006, and June 30, 2011, were included if they had a cranial ultrasonogram performed prior to 36 weeks’ postmenstrual age. Comparisons were made between those with ventriculomegaly and those with normal cranial sonograms. Data analysis was completed from August 2013 to August 2017. Main Outcomes and Measures The main outcome was neurodevelopmental impairment, defined as a Bayley Scales of Infant and Toddler Development III cognitive score less than 70, moderate/severe cerebral palsy, a Gross Motor Function Classification System score of level 2 or more, vision impairment, or hearing impairment. Secondary outcomes included Bayley Scales of Infant and Toddler Development III subscores, components of neurodevelopmental impairment, behavioral outcomes, and death/neurodevelopmental impairment. Logistic regression was used to evaluate the association of ventriculomegaly with adverse outcomes while controlling for potentially confounding variables and center differences as a random effect. Linear regression was used similarly for continuous outcomes. Results Of 4193 neonates with ultrasonography data, 300 had nonhemorrhagic ventriculomegaly (7%); 3045 had normal cranial ultrasonograms (73%), 775 had periventricular-intraventricular hemorrhage (18.5%), and 73 had cystic periventricular leukomalacia (1.7%). Outcomes were available for 3008 of 3345 neonates with ventriculomegaly or normal scans (90%). Compared with normal cranial ultrasonograms, ventriculomegaly was associated with lower gestational age, male sex, and bronchopulmonary dysplasia, late-onset sepsis, meningitis, necrotizing enterocolitis, and stage 3 retinopathy of prematurity. After adjustment, neonates with ventriculomegaly had higher odds of neurodevelopmental impairment (odds ratio [OR], 3.07; 95% CI, 2.13-4.43), cognitive impairment (OR, 3.23; 95% CI, 2.09-4.99), moderate/severe cerebral palsy (OR, 3.68; 95% CI, 2.08-6.51), death/neurodevelopmental impairment (OR, 2.17; 95% CI, 1.62-2.91), but not death alone (OR, 1.09; 95% CI, 0.76-1.57). Behavioral outcomes did not differ. Conclusions and Relevance Nonhemorrhagic ventriculomegaly is associated with increased odds of neurodevelopmental impairment among extremely preterm neonates.
中文翻译:

在没有脑室周围-脑室内出血的情况下患有脑室扩大的极早产儿的神经发育和行为结果
对极早产儿队列的颅超声检查和儿童早期结局的研究表明,脑室周围-脑室内出血和囊性脑室周围白质软化与不良的神经发育结果有关。然而,尚未完全了解非出血性脑室扩大与神经发育和行为结果之间的关联。目的 表征小于 27 周胎龄的极早产儿的结局,这些新生儿经历了在 36 周后经期前检测到的非出血性脑室扩大。设计、设置和参与者 这项纵向观察研究是在尤尼斯·肯尼迪·施莱佛国家儿童健康与人类发展研究所新生儿研究网络的 16 个中心进行的。2006 年 7 月 1 日至 2011 年 6 月 30 日期间在任何网络设施中出生 27 周之前出生的婴儿,如果他们在月经后 36 周之前进行了颅脑超声检查,则包括在内。将脑室扩大者与颅脑超声检查正常者进行比较。数据分析于2013年8月至2017年8月完成。 主要结果和措施主要结果是神经发育障碍,定义为贝利婴幼儿发育量表III认知评分低于70,中/重度脑瘫,粗大运动功能分类系统评分 2 级或以上、视力障碍或听力障碍。次要结果包括贝利婴幼儿发展量表 III 子评分、神经发育障碍的组成部分、行为结果、和死亡/神经发育障碍。Logistic 回归用于评估脑室扩大与不良结果的关联,同时控制潜在的混杂变量和中心差异作为随机效应。线性回归类似地用于连续结果。结果 4193例有超声检查数据的新生儿中,300例有非出血性脑室扩大(7%);3045 例颅脑超声检查正常 (73%),775 例脑室周围-脑室内出血 (18.5%),73 例囊性脑室周围白质软化 (1.7%)。3345 名患有脑室扩大或正常扫描的新生儿中的 3008 名 (90%) 可获得结果。与正常颅脑超声检查相比,脑室扩大与低胎龄、男性、支气管肺发育不良、迟发性败血症、脑膜炎、坏死性小肠结肠炎和早产儿 3 期视网膜病变。调整后,脑室扩大的新生儿出现神经发育障碍(OR 3.07;95% CI 2.13-4.43)、认知障碍(OR 3.23;95% CI 2.09-4.99)、中/重度脑麻痹(OR,3.68;95% CI,2.08-6.51),死亡/神经发育障碍(OR,2.17;95% CI,1.62-2.91),但不单独死亡(OR,1.09;95% CI,0.76-1.57) . 行为结果没有不同。结论和相关性 非出血性脑室扩大与极早产儿神经发育障碍的几率增加有关。2.09-4.99),中度/重度脑瘫(OR,3.68;95% CI,2.08-6.51),死亡/神经发育障碍(OR,2.17;95% CI,1.62-2.91),但不单独死亡(OR,1.09) ;95% CI,0.76-1.57)。行为结果没有不同。结论和相关性 非出血性脑室扩大与极早产儿神经发育障碍的几率增加有关。2.09-4.99),中度/重度脑瘫(OR,3.68;95% CI,2.08-6.51),死亡/神经发育障碍(OR,2.17;95% CI,1.62-2.91),但不单独死亡(OR,1.09) ;95% CI,0.76-1.57)。行为结果没有不同。结论和相关性 非出血性脑室扩大与极早产儿神经发育障碍的几率增加有关。
更新日期:2018-01-01
中文翻译:

在没有脑室周围-脑室内出血的情况下患有脑室扩大的极早产儿的神经发育和行为结果
对极早产儿队列的颅超声检查和儿童早期结局的研究表明,脑室周围-脑室内出血和囊性脑室周围白质软化与不良的神经发育结果有关。然而,尚未完全了解非出血性脑室扩大与神经发育和行为结果之间的关联。目的 表征小于 27 周胎龄的极早产儿的结局,这些新生儿经历了在 36 周后经期前检测到的非出血性脑室扩大。设计、设置和参与者 这项纵向观察研究是在尤尼斯·肯尼迪·施莱佛国家儿童健康与人类发展研究所新生儿研究网络的 16 个中心进行的。2006 年 7 月 1 日至 2011 年 6 月 30 日期间在任何网络设施中出生 27 周之前出生的婴儿,如果他们在月经后 36 周之前进行了颅脑超声检查,则包括在内。将脑室扩大者与颅脑超声检查正常者进行比较。数据分析于2013年8月至2017年8月完成。 主要结果和措施主要结果是神经发育障碍,定义为贝利婴幼儿发育量表III认知评分低于70,中/重度脑瘫,粗大运动功能分类系统评分 2 级或以上、视力障碍或听力障碍。次要结果包括贝利婴幼儿发展量表 III 子评分、神经发育障碍的组成部分、行为结果、和死亡/神经发育障碍。Logistic 回归用于评估脑室扩大与不良结果的关联,同时控制潜在的混杂变量和中心差异作为随机效应。线性回归类似地用于连续结果。结果 4193例有超声检查数据的新生儿中,300例有非出血性脑室扩大(7%);3045 例颅脑超声检查正常 (73%),775 例脑室周围-脑室内出血 (18.5%),73 例囊性脑室周围白质软化 (1.7%)。3345 名患有脑室扩大或正常扫描的新生儿中的 3008 名 (90%) 可获得结果。与正常颅脑超声检查相比,脑室扩大与低胎龄、男性、支气管肺发育不良、迟发性败血症、脑膜炎、坏死性小肠结肠炎和早产儿 3 期视网膜病变。调整后,脑室扩大的新生儿出现神经发育障碍(OR 3.07;95% CI 2.13-4.43)、认知障碍(OR 3.23;95% CI 2.09-4.99)、中/重度脑麻痹(OR,3.68;95% CI,2.08-6.51),死亡/神经发育障碍(OR,2.17;95% CI,1.62-2.91),但不单独死亡(OR,1.09;95% CI,0.76-1.57) . 行为结果没有不同。结论和相关性 非出血性脑室扩大与极早产儿神经发育障碍的几率增加有关。2.09-4.99),中度/重度脑瘫(OR,3.68;95% CI,2.08-6.51),死亡/神经发育障碍(OR,2.17;95% CI,1.62-2.91),但不单独死亡(OR,1.09) ;95% CI,0.76-1.57)。行为结果没有不同。结论和相关性 非出血性脑室扩大与极早产儿神经发育障碍的几率增加有关。2.09-4.99),中度/重度脑瘫(OR,3.68;95% CI,2.08-6.51),死亡/神经发育障碍(OR,2.17;95% CI,1.62-2.91),但不单独死亡(OR,1.09) ;95% CI,0.76-1.57)。行为结果没有不同。结论和相关性 非出血性脑室扩大与极早产儿神经发育障碍的几率增加有关。



























 京公网安备 11010802027423号
京公网安备 11010802027423号