PLOS Medicine ( IF 10.5 ) Pub Date : 2017-11-21 , DOI: 10.1371/journal.pmed.1002444 Robyn Eakle , Gabriela B. Gomez , Niven Naicker , Rutendo Bothma , Judie Mbogua , Maria A. Cabrera Escobar , Elaine Saayman , Michelle Moorhouse , W. D. Francois Venter , Helen Rees ,
|
Background
Operational research is required to design delivery of pre-exposure prophylaxis (PrEP) and early antiretroviral treatment (ART). This paper presents the primary analysis of programmatic data, as well as demographic, behavioural, and clinical data, from the TAPS Demonstration Project, which offered both interventions to female sex workers (FSWs) at 2 urban clinic sites in South Africa.
Methods and findings
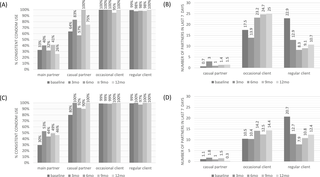
The TAPS study was conducted between 30 March 2015 and 30 June 2017, with the enrolment period ending on 31 July 2016. TAPS was a prospective observational cohort study with 2 groups receiving interventions delivered in existing service settings: (1) PrEP as part of combination prevention for HIV-negative FSWs and (2) early ART for HIV-positive FSWs. The main outcome was programme retention at 12 months of follow-up. Of the 947 FSWs initially seen in clinic, 692 were HIV tested. HIV prevalence was 49%. Among those returning to clinic after HIV testing and clinical screening, 93% of the women who were HIV-negative were confirmed as clinically eligible for PrEP (n = 224/241), and 41% (n = 110/270) of the women who were HIV-positive had CD4 counts within National Department of Health ART initiation guidelines at assessment. Of the remaining women who were HIV-positive, 93% were eligible for early ART (n = 148/160). From those eligible, 98% (n = 219/224) and 94% (n = 139/148) took up PrEP and early ART, respectively. At baseline, a substantial fraction of women had a steady partner, worked in brothels, and were born in Zimbabwe. Of those enrolled, 22% on PrEP (n = 49/219) and 60% on early ART (n = 83/139) were seen at 12 months; we observed high rates of loss to follow-up: 71% (n = 156/219) and 30% (n = 42/139) in the PrEP and early ART groups, respectively. Little change over time was reported in consistent condom use or the number of sexual partners in the last 7 days, with high levels of consistent condom use with clients and low use with steady partners in both study groups. There were no seroconversions on PrEP and 7 virological failures on early ART among women remaining in the study. Reported adherence to PrEP varied over time between 70% and 85%, whereas over 90% of participants reported taking pills daily while on early ART. Data on provider-side costs were also collected and analysed. The total cost of service delivery was approximately US$126 for PrEP and US$406 for early ART per person-year. The main limitations of this study include the lack of a control group, which was not included due to ethical considerations; clinical study requirements imposed when PrEP was not approved through the regulatory system, which could have affected uptake; and the timing of the implementation of a national sex worker HIV programme, which could have also affected uptake and retention.
Conclusions
PrEP and early ART services can be implemented within FSW routine services in high prevalence, urban settings. We observed good uptake for both PrEP and early ART; however, retention rates for PrEP were low. Retention rates for early ART were similar to retention rates for the current standard of care. While the cost of the interventions was higher than previously published, there is potential for cost reduction at scale. The TAPS Demonstration Project results provided the basis for the first government PrEP and early ART guidelines and the rollout of the national sex worker HIV programme in South Africa.
中文翻译:

南非女性性工作者中的HIV暴露前预防和早期抗逆转录病毒治疗:一项前瞻性观察示范项目的结果
背景
需要进行运筹学研究,以设计暴露前预防措施(PrEP)和早期抗逆转录病毒治疗(ART)的交付方式。本文介绍了来自TAPS示范项目的程序化数据以及人口统计,行为和临床数据的主要分析,该项目为南非2个城市诊所的女性性工作者(FSW)提供了两种干预措施。
方法和发现
TAPS研究于2015年3月30日至2017年6月30日进行,招募期于2016年7月31日结束。TAPS是一项前瞻性观察性队列研究,有2个小组在现有服务环境中接受干预:(1)PrEP作为合并的一部分预防HIV阴性FSW和(2)早期ART预防HIV阳性FSW。主要结果是在随访的12个月中保留了程序。最初在诊所看到的947名FSW中,有692名接受了HIV检测。HIV感染率为49%。在经过HIV检测和临床筛查后返回诊所的患者中,有93%的HIV阴性女性被确认具有临床上的PrEP资格(n = 224/241),有41%(n =在评估中,HIV阳性女性中有110/270)的CD4计数在美国国家卫生部ART起始指南中。在其余的HIV阳性妇女中,有93%有资格进行早期抗逆转录病毒治疗(n = 148/160)。在符合条件的患者中,分别有98%(n = 219/224)和94%(n = 139/148)接受了PrEP和早期ART。在基线时,很大一部分妇女有稳定的伴侣,在妓院工作,并出生在津巴布韦。在入组的12个月时,有22%的PrEP患者(n = 49/219)和60%的早期ART患者(n = 83/139)。我们观察到随访失误率很高:71%(n = 156/219)和30%(n =PrEP组和早期ART组分别为42/139)。在过去的7天中,持续使用安全套或性伴侣的数量随时间变化几乎没有变化,两个研究组中与顾客保持一致的安全套使用率较高,而与稳定伴侣的使用率较低。该研究中剩余的女性在PrEP上没有血清转化,在早期ART上没有7病毒学衰竭。报告的对PrEP的依从性随时间的变化在70%到85%之间,而超过90%的参与者报告在早期ART期间每天服用药丸。还收集并分析了提供方成本的数据。PrEP服务交付的总成本约为每人年126美元,早期抗病毒治疗的成本为406美元。这项研究的主要局限性包括缺乏对照组,出于伦理考虑,该对照组未包括在内;当PrEP未通过监管系统批准时可能施加的临床研究要求,这可能会影响摄入量;以及实施国家性工作者艾滋病毒计划的时间,这也可能影响吸收和保留。
结论
PrEP和早期ART服务可以在流行率较高的城市环境中的FSW常规服务中实施。我们观察到PrEP和早期ART均具有良好的摄取。但是,PrEP的保留率很低。早期ART的保留率与当前护理标准的保留率相似。尽管干预措施的成本比以前公布的要高,但有可能大规模降低成本。TAPS示范项目的结果为第一个政府PrEP和早期ART指南以及在南非推出全国性工作者HIV计划提供了基础。











































 京公网安备 11010802027423号
京公网安备 11010802027423号