PLOS Neglected Tropical Diseases ( IF 3.4 ) Pub Date : 2017-11-20 , DOI: 10.1371/journal.pntd.0006094 Romain Guery , Benoit Henry , Guillaume Martin-Blondel , Claire Rouzaud , Florence Cordoliani , Gundel Harms , Jean-Pierre Gangneux , Françoise Foulet , Emmanuelle Bourrat , Michel Baccard , Gloria Morizot , Paul-Henri Consigny , Antoine Berry , Johannes Blum , Olivier Lortholary , Pierre Buffet ,
|
Background
Complex cutaneous and muco-cutaneous leishmaniasis (CL and MCL) often requires systemic therapy. Liposomal amphotericin B (L-AmB) has a strong potential for a solid clinical benefit in this indication.
Methods
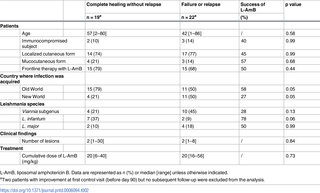
We conducted a retrospective analysis of data from a French centralized referral treatment program and from the “LeishMan” European consortium database. All patients with parasitologically proven CL or MCL who received at least one dose of L-AmB were included. Positive outcome was based on ulcer closure as per recent WHO workshop guidelines.
Results
From 2008 through 2016, 43 travelers returning from 18 countries (Old World n = 28; New World n = 15) were analyzed with a median follow-up duration of 79 days [range 28–803]. Main clinical forms were: localized CL with one or multiple lesions (n = 32; 74%) and MCL (n = 8; 19%). As per published criteria 19 of 41 patients (46%) were cured 90 days after one course of L-AmB. When the following items -improvement before day 90 but no subsequent follow-up, delayed healing (>3 months) and healing after a second course of L-AmB- were included in the definition of cure, 27 of 43 patients (63%) had a positive outcome. Five patients (MCL = 1; CL = 4) experienced a relapse after a median duration of 6 months [range 3–27] post treatment and 53% of patients (23/43) experienced at least one adverse event including severe hypokalaemia and acute cardiac failure (one patient each). In multivariate analysis, tegumentary infection with L. infantum was associated with complete healing after L-AmB therapy (OR 5.8 IC 95% [1.03–32]) while infection with other species had no impact on outcome.
Conclusion
In conditions close to current medical practice, the therapeutic window of L-AmB was narrow in travellers with CL or MCL, with the possible exception of those infected with L. infantum. Strict follow-up is warranted when using L-AmB in patients with mild disease.
中文翻译:

患有皮肤和粘膜皮肤利什曼病的旅行者中的脂质体两性霉素B:不是万能药
背景
复杂的皮肤和粘膜皮肤利什曼病(CL和MCL)通常需要全身治疗。脂质体两性霉素B(L-AmB)具有很强的潜力,可在此适应症中获得可靠的临床益处。
方法
我们对法国集中转诊治疗计划和“ LeishMan”欧洲联盟数据库的数据进行了回顾性分析。包括所有接受至少一剂L-AmB的寄生虫学证实的CL或MCL的患者。根据最近的世界卫生组织讲习班指南,积极的结果是基于溃疡的闭合。
结果
从2008年到2016年,对来自18个国家(旧世界n = 28;新世界n = 15)返回的43位旅行者进行了分析,中位随访时间为79天[范围28-803]。主要临床形式为:具有一个或多个病变的局部CL(n = 32; 74%)和MCL(n = 8; 19%)。根据公布的标准,一疗程的L-AmB治疗90天后,有41位患者中的19位(46%)治愈了。如果以下定义-在第90天之前有所改善,但没有随后的随访,延迟的愈合(> 3个月)和第二个L-AmB疗程后的愈合被包括在治愈的定义中,则43例患者中有27例(63%)取得了积极的成果。五名患者(MCL = 1; CL = 4)治疗后中位时间6个月[范围3–27]后经历了复发,并且53%的患者(23/43)经历了至少一种不良事件,包括严重的低钾血症和急性心力衰竭(每例一名患者) 。在多变量分析中,大号。L-AmB治疗后婴儿与完全愈合相关(OR 5.8 IC 95%[1.03-32]),而其他物种的感染对结局没有影响。
结论
在接近当前医学实践的情况下,CL或MCL旅行者的L-AmB的治疗范围较窄,可能感染L的患者除外。婴儿的。在轻度疾病患者中使用L-AmB时,应严格随访。











































 京公网安备 11010802027423号
京公网安备 11010802027423号