当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Care Planning for Inpatients Referred for Palliative Care Consultation
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2018-01-01 , DOI: 10.1001/jamainternmed.2017.6313 Kara Bischoff 1 , David L. O’Riordan 1 , Angela K. Marks 1 , Rebecca Sudore 2, 3 , Steven Z. Pantilat 1
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2018-01-01 , DOI: 10.1001/jamainternmed.2017.6313 Kara Bischoff 1 , David L. O’Riordan 1 , Angela K. Marks 1 , Rebecca Sudore 2, 3 , Steven Z. Pantilat 1
Affiliation
|
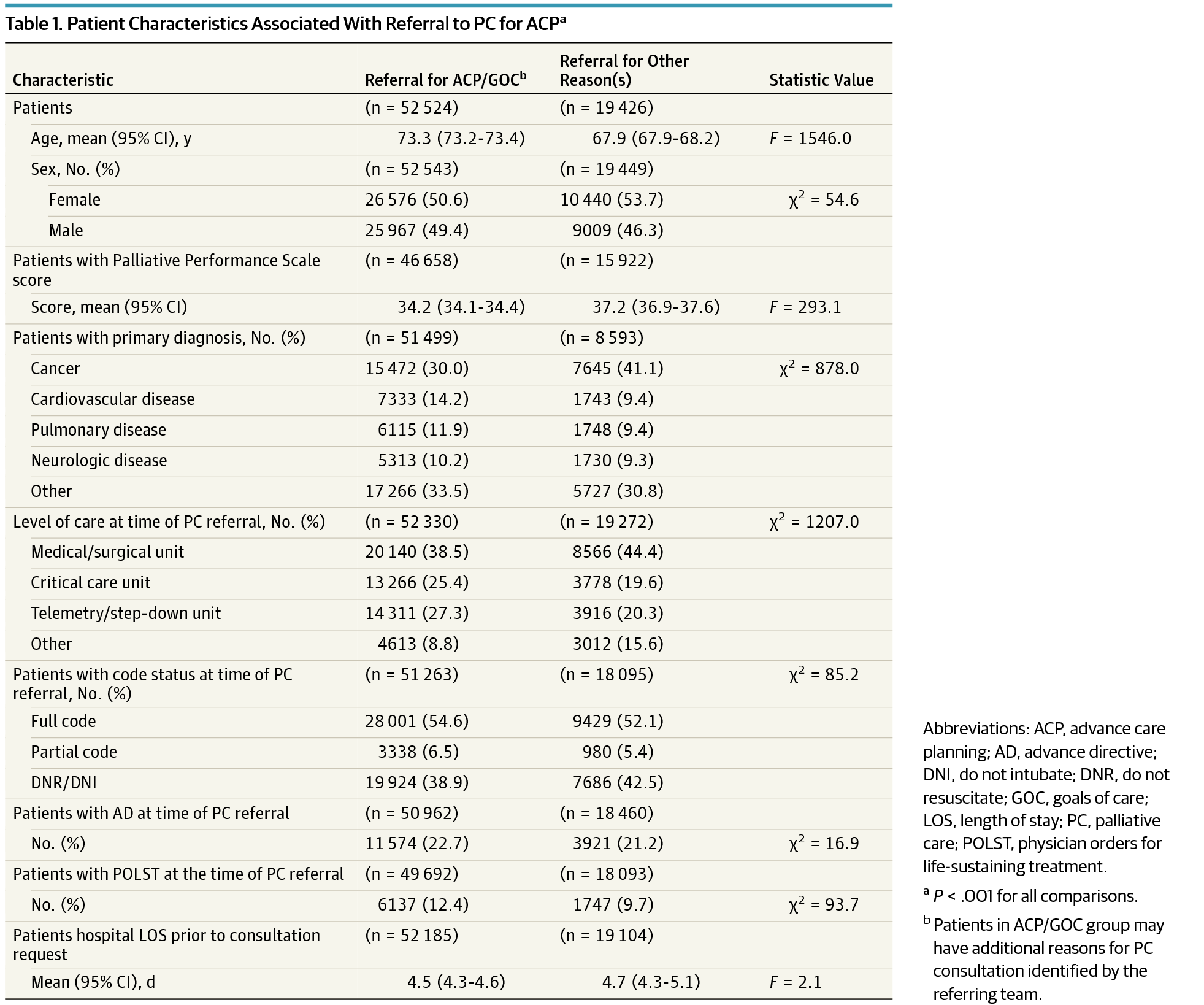
Importance Care planning is a critical function of palliative care teams, but the impact of advance care planning and goals of care discussions by palliative care teams has not been well characterized. Objective To describe the population of patients referred to inpatient palliative care consultation teams for care planning, the needs identified by palliative care clinicians, the care planning activities that occur, and the results of these activities. Design, Setting, and Participants This was a prospective cohort study conducted between January 1, 2013, and December 31, 2016. Seventy-eight inpatient palliative care teams from diverse US hospitals in the Palliative Care Quality Network, a national quality improvement collaborative. Standardized data were submitted for 73 145 patients. Exposures Inpatient palliative care consultation. Results Overall, 52 571 of 73 145 patients (71.9%) referred to inpatient palliative care were referred for care planning (range among teams, 27.5%-99.4% of patients). Patients referred for care planning were older (73.3 vs 67.9 years; F statistic, 1546.0; P < .001), less likely to have cancer (30.0% vs 41.1%; P < .001), and slightly more often had a clinical order of full code at the time of referral (54.6% vs 52.1%; P < .001). Palliative care teams identified care planning needs in 52 825 of 73 145 patients (72.2%) overall, including 42 467 of 49 713 patients (85.4%) referred for care planning and in 10 054 of 17 475 patients (57.5%) referred for other reasons. Through care planning conversations, surrogates were identified for 10 571 of 11 149 patients (94.8%) and 9026 patients (37.4%) elected to change their code status. Substantially more patients indicated that a status of do not resuscitate/do not intubate was consistent with their goals (7006 [32.1%] preconsultation to 13 773 [63.1%] postconsultation). However, an advance directive was completed for just 2160 of 67 955 patients (3.2%) and a Physicians Orders for Life-Sustaining Treatment form was completed for 8359 of 67 955 patients (12.3%) seen by palliative care teams. Conclusions and Relevance Care planning was the most common reason for inpatient palliative care consultation, and care planning needs were often found even when the consultation was for other reasons. Surrogates were consistently identified, and patients’ preferences regarding life-sustaining treatments were frequently updated. However, a minority of patients completed legal forms to document their care preferences, highlighting an area in need of improvement.
中文翻译:

转介进行姑息治疗咨询的住院病人的护理计划
重要性 护理计划是姑息护理团队的一项重要职能,但姑息护理团队的预先护理计划和护理讨论目标的影响尚未得到很好的描述。目的 描述转诊至住院姑息治疗咨询团队进行护理计划的患者群体、姑息护理临床医生确定的需求、发生的护理计划活动以及这些活动的结果。设计、设置和参与者 这是一项前瞻性队列研究,于 2013 年 1 月 1 日至 2016 年 12 月 31 日期间进行。来自美国不同医院的 78 个住院姑息治疗团队参与了姑息治疗质量网络,这是一个全国质量改进合作组织。提交了 73 145 名患者的标准化数据。暴露 住院姑息治疗咨询。结果 总体而言,转诊至住院姑息治疗的 73 145 名患者中有 52 571 名 (71.9%) 被转诊进行护理计划(各团队之间,27.5%-99.4% 的患者)。转诊进行护理计划的患者年龄较大(73.3 岁与 67.9 岁;F 统计量,1546.0;P < .001),患癌症的可能性较小(30.0% 与 41.1%;P < .001),并且有临床订单的频率略高转诊时的完整代码(54.6% 对 52.1%;P < .001)。姑息治疗团队确定了 73 145 名患者中的 52 825 名(72.2%)的护理计划需求,包括转诊至护理计划的 49 713 名患者中的 42 467 名(85.4%)和转诊至其他患者的 17 475 名患者中的 10 054 名(57.5%)原因。通过护理计划对话,确定了 11 149 名患者中的 10 571 名 (94.8%) 和 9026 名选择更改其代码状态的患者 (37.4%) 的代理人。相当多的患者表示不复苏/不插管的状态符合他们的目标(7006 [32.1%] 会诊前到 13 773 [63.1%] 会诊后)。然而,仅有 67 955 名患者中的 2160 名(3.2%)完成了预先指示,而姑息治疗团队就诊的 67 955 名患者中的 8359 名(12.3%)完成了生命维持治疗的医师医嘱表。结论和相关性 护理计划是住院姑息治疗咨询的最常见原因,即使咨询是出于其他原因,也经常发现护理计划需求。不断地确定替代物,并且经常更新患者对维持生命治疗的偏好。然而,少数患者填写了法律表格来记录他们的护理偏好,
更新日期:2018-01-01
中文翻译:

转介进行姑息治疗咨询的住院病人的护理计划
重要性 护理计划是姑息护理团队的一项重要职能,但姑息护理团队的预先护理计划和护理讨论目标的影响尚未得到很好的描述。目的 描述转诊至住院姑息治疗咨询团队进行护理计划的患者群体、姑息护理临床医生确定的需求、发生的护理计划活动以及这些活动的结果。设计、设置和参与者 这是一项前瞻性队列研究,于 2013 年 1 月 1 日至 2016 年 12 月 31 日期间进行。来自美国不同医院的 78 个住院姑息治疗团队参与了姑息治疗质量网络,这是一个全国质量改进合作组织。提交了 73 145 名患者的标准化数据。暴露 住院姑息治疗咨询。结果 总体而言,转诊至住院姑息治疗的 73 145 名患者中有 52 571 名 (71.9%) 被转诊进行护理计划(各团队之间,27.5%-99.4% 的患者)。转诊进行护理计划的患者年龄较大(73.3 岁与 67.9 岁;F 统计量,1546.0;P < .001),患癌症的可能性较小(30.0% 与 41.1%;P < .001),并且有临床订单的频率略高转诊时的完整代码(54.6% 对 52.1%;P < .001)。姑息治疗团队确定了 73 145 名患者中的 52 825 名(72.2%)的护理计划需求,包括转诊至护理计划的 49 713 名患者中的 42 467 名(85.4%)和转诊至其他患者的 17 475 名患者中的 10 054 名(57.5%)原因。通过护理计划对话,确定了 11 149 名患者中的 10 571 名 (94.8%) 和 9026 名选择更改其代码状态的患者 (37.4%) 的代理人。相当多的患者表示不复苏/不插管的状态符合他们的目标(7006 [32.1%] 会诊前到 13 773 [63.1%] 会诊后)。然而,仅有 67 955 名患者中的 2160 名(3.2%)完成了预先指示,而姑息治疗团队就诊的 67 955 名患者中的 8359 名(12.3%)完成了生命维持治疗的医师医嘱表。结论和相关性 护理计划是住院姑息治疗咨询的最常见原因,即使咨询是出于其他原因,也经常发现护理计划需求。不断地确定替代物,并且经常更新患者对维持生命治疗的偏好。然而,少数患者填写了法律表格来记录他们的护理偏好,











































 京公网安备 11010802027423号
京公网安备 11010802027423号