PLOS Neglected Tropical Diseases ( IF 3.8 ) Pub Date : 2017-10-26 , DOI: 10.1371/journal.pntd.0005985 Christopher Fitzpatrick 1 , Kingsley Asiedu 1 , Anita Sands 1 , Tita Gonzalez Pena 1, 2 , Michael Marks 3 , Oriol Mitja 4 , Filip Meheus 5, 6 , Patrick Van der Stuyft 7, 8
|
Background
Yaws is a non-venereal treponemal infection caused by Treponema pallidum subspecies pertenue. The disease is targeted by WHO for eradication by 2020. Rapid diagnostic tests (RDTs) are envisaged for confirmation of clinical cases during treatment campaigns and for certification of the interruption of transmission. Yaws testing requires both treponemal (trep) and non-treponemal (non-trep) assays for diagnosis of current infection. We evaluate a sequential testing strategy (using a treponemal RDT before a trep/non-trep RDT) in terms of cost and cost-effectiveness, relative to a single-assay combined testing strategy (using the trep/non-trep RDT alone), for two use cases: individual diagnosis and community surveillance.
Methods
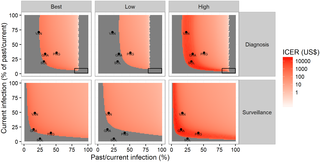
We use cohort decision analysis to examine the diagnostic and cost outcomes. We estimate cost and cost-effectiveness of the alternative testing strategies at different levels of prevalence of past/current infection and current infection under each use case. We take the perspective of the global yaws eradication programme. We calculate the total number of correct diagnoses for each strategy over a range of plausible prevalences. We employ probabilistic sensitivity analysis (PSA) to account for uncertainty and report 95% intervals.
Results
At current prices of the treponemal and trep/non-trep RDTs, the sequential strategy is cost-saving for individual diagnosis at prevalence of past/current infection less than 85% (81–90); it is cost-saving for surveillance at less than 100%. The threshold price of the trep/non-trep RDT (below which the sequential strategy would no longer be cost-saving) is US$ 1.08 (1.02–1.14) for individual diagnosis at high prevalence of past/current infection (51%) and US$ 0.54 (0.52–0.56) for community surveillance at low prevalence (15%).
Discussion
We find that the sequential strategy is cost-saving for both diagnosis and surveillance in most relevant settings. In the absence of evidence assessing relative performance (sensitivity and specificity), cost-effectiveness is uncertain. However, the conditions under which the combined test only strategy might be more cost-effective than the sequential strategy are limited. A cheaper trep/non-trep RDT is needed, costing no more than US$ 0.50–1.00, depending on the use case. Our results will help enhance the cost-effectiveness of yaws programmes in the 13 countries known to be currently endemic. It will also inform efforts in the much larger group of 71 countries with a history of yaws, many of which will have to undertake surveillance to confirm the interruption of transmission.
中文翻译:

用于偏航诊断和监测的快速测试策略的成本和成本效益
背景
雅司病是由梅毒螺旋体亚种永久感染引起的一种非性病密螺旋体感染。世卫组织的目标是到 2020 年根除该疾病。设想快速诊断测试 (RDT) 用于在治疗活动期间确认临床病例并证明传播中断。雅司病检测需要密螺旋体 (trep) 和非密螺旋体 (non-trep) 检测来诊断当前感染。我们在成本和成本效益方面评估顺序测试策略(在 Trep/非 Trep RDT 之前使用密螺旋体 RDT),相对于单次检测组合测试策略(单独使用 Trep/非 Trep RDT),用于两个用例:个人诊断和社区监测。
方法
我们使用队列决策分析来检查诊断和成本结果。我们在每个用例下估计了过去/当前感染和当前感染的不同流行水平下替代测试策略的成本和成本效益。我们从全球雅司病根除计划的角度出发。我们计算了在一系列可能的流行范围内每种策略的正确诊断总数。我们采用概率敏感性分析 (PSA) 来解释不确定性并报告 95% 的区间。
结果
以密螺旋体和密螺旋体/非密螺旋体 RDT 的当前价格,在过去/当前感染率低于 85% (81-90) 的情况下,序贯策略可以节省个体诊断的成本;监控成本节省不到 100%。在过去/当前感染高流行率 (51%) 和低流行率 (15%) 的社区监测 0.54 美元 (0.52–0.56)。
讨论
我们发现,在大多数相关环境中,顺序策略对于诊断和监测都可以节省成本。在缺乏评估相对性能(敏感性和特异性)的证据的情况下,成本效益是不确定的。但是,仅组合测试策略可能比顺序策略更具成本效益的条件是有限的。需要更便宜的 Trep/非 Trep RDT,成本不超过 0.50-1.00 美元,具体取决于用例。我们的研究结果将有助于提高 13 个目前流行的雅司病项目的成本效益。它还将为更大范围的 71 个有雅司病史的国家的工作提供信息,其中许多国家将不得不进行监测以确认传播中断。



























 京公网安备 11010802027423号
京公网安备 11010802027423号