当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
The contribution of alcohol-use disorder to decompensated cirrhosis among people with hepatitis C: an international study
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-03-01 , DOI: 10.1016/j.jhep.2017.10.019 Maryam Alavi , Naveed Z. Janjua , Mei Chong , Jason Grebely , Esther J. Aspinall , Hamish Innes , Heather M. Valerio , Behzad Hajarizadeh , Peter C. Hayes , Mel Krajden , Janaki Amin , Matthew G. Law , Jacob George , David J. Goldberg , Sharon J. Hutchinson , Gregory J. Dore
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-03-01 , DOI: 10.1016/j.jhep.2017.10.019 Maryam Alavi , Naveed Z. Janjua , Mei Chong , Jason Grebely , Esther J. Aspinall , Hamish Innes , Heather M. Valerio , Behzad Hajarizadeh , Peter C. Hayes , Mel Krajden , Janaki Amin , Matthew G. Law , Jacob George , David J. Goldberg , Sharon J. Hutchinson , Gregory J. Dore
|
BACKGROUND & AIMS
The advent of direct-acting antivirals (DAAs) has led to ambitious targets for hepatitis C virus (HCV) elimination. However, in the context of alcohol use disorder the ability of DAAs to achieve these targets may be compromised. The aim of this study was to evaluate the contribution of alcohol use disorder to HCV-related decompensated cirrhosis in three settings. METHODS
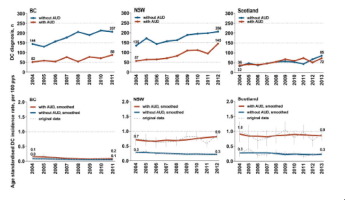
HCV notifications from British Columbia, Canada; New South Wales, Australia, and Scotland (1995-2011/2012/2013, respectively) were linked to hospital admissions (2001-2012/2013/2014, respectively). Alcohol use disorder was defined as non-liver-related hospitalisation due to alcohol use. Age-standardised decompensated cirrhosis incidence rates were plotted, associated factors were assessed using Cox regression, and alcohol use disorder-associated population attributable fractions (PAFs) were computed. RESULTS
Among 58,487, 84,529, and 31,924 people with HCV in British Columbia, New South Wales, and Scotland, 2,689 (4.6%), 3,169 (3.7%), and 1,375 (4.3%) had a decompensated cirrhosis diagnosis, and 28%, 32%, and 50% of those with decompensated cirrhosis had an alcohol use disorder, respectively. Age-standardised decompensated cirrhosis incidence rates were considerably higher in people with alcohol use disorder in New South Wales and Scotland. Decompensated cirrhosis was independently associated with alcohol use disorder in British Columbia (aHR 1.92; 95% CI 1.76-2.10), New South Wales (aHR 3.68; 95% CI 3.38-4.00) and Scotland (aHR 3.88; 95% CI 3.42-4.40). The PAFs of decompensated cirrhosis-related to alcohol use disorder were 13%, 25%, and 40% in British Columbia, New South Wales and Scotland, respectively. CONCLUSIONS
Alcohol use disorder was a major contributor to HCV liver disease burden in all settings, more distinctly in Scotland. The extent to which alcohol use would compromise the individual and population-level benefits of DAA therapy needs to be closely monitored. Countries, where appropriate, must develop strategies combining promotion of DAA treatment uptake with management of alcohol use disorders, if World Health Organization 2030 HCV mortality reduction targets are going to be achieved. LAY SUMMARY
The burden of liver disease has been rising among people with hepatitis C globally. The recent introduction of highly effective medicines against hepatitis C (called direct-acting antivirals or DAAs) has brought renewed optimism to the sector. DAA scale-up could eliminate hepatitis C as a public health threat in the coming decades. However, our findings show heavy alcohol use is a major risk factor for liver disease among people with hepatitis C. If continued, heavy alcohol use could compromise the benefits of new antiviral treatments at the individual- and population-level. To tackle hepatitis C as a public health threat, where needed, DAA therapy should be combined with management of heavy alcohol use.
中文翻译:

酒精使用障碍对丙型肝炎患者失代偿期肝硬化的影响:一项国际研究
背景与目标 直接作用抗病毒药物 (DAA) 的出现已经为消除丙型肝炎病毒 (HCV) 制定了雄心勃勃的目标。然而,在酒精使用障碍的情况下,DAAs 实现这些目标的能力可能会受到影响。本研究的目的是评估酒精使用障碍在三种情况下对 HCV 相关失代偿性肝硬化的影响。方法 来自加拿大不列颠哥伦比亚省的 HCV 通报;新南威尔士州、澳大利亚和苏格兰(分别为 1995-2011/2012/2013)与住院(分别为 2001-2012/2013/2014)有关。酒精使用障碍被定义为因酒精使用而与肝脏无关的住院治疗。绘制了年龄标准化的失代偿期肝硬化发病率,使用 Cox 回归评估相关因素,和酒精使用障碍相关的人口归因分数(PAF)被计算出来。结果 在不列颠哥伦比亚、新南威尔士和苏格兰的 58,487、84,529 和 31,924 名 HCV 患者中,2,689 (4.6%)、3,169 (3.7%) 和 1,375 (4.3%) 有失代偿期肝硬化,诊断为 28% 32% 和 50% 的失代偿性肝硬化患者分别有酒精使用障碍。在新南威尔士州和苏格兰,酒精使用障碍患者的年龄标准化失代偿性肝硬化发病率要高得多。在不列颠哥伦比亚省 (aHR 1.92; 95% CI 1.76-2.10)、新南威尔士州 (aHR 3.68; 95% CI 3.38-4.00) 和苏格兰 (aHR 3.88; 95% CI 3.42-4.40),失代偿期肝硬化与酒精使用障碍独立相关)。与酒精使用障碍相关的失代偿期肝硬化的 PAF 分别为 13%、25%、不列颠哥伦比亚省、新南威尔士州和苏格兰分别为 40%。结论 酒精使用障碍是所有环境中 HCV 肝病负担的主要因素,在苏格兰更为明显。需要密切监测酒精使用会在多大程度上损害 DAA 治疗的个人和人群水平的益处。如果要实现世界卫生组织 2030 年降低 HCV 死亡率的目标,各国必须在适当的情况下制定战略,将促进 DAA 治疗与管理酒精使用障碍相结合。概述 全球丙型肝炎患者的肝脏疾病负担一直在增加。最近推出的针对丙型肝炎的高效药物(称为直接作用抗病毒药物或 DAA)为该行业带来了新的乐观情绪。DAA 的扩大可以消除丙型肝炎作为未来几十年的公共卫生威胁。然而,我们的研究结果表明,大量饮酒是丙型肝炎患者肝病的主要危险因素。如果继续,大量饮酒可能会损害新的抗病毒治疗在个人和人群层面的益处。为了在需要时将丙型肝炎作为公共卫生威胁来应对,DAA 治疗应与重度饮酒管理相结合。
更新日期:2018-03-01
中文翻译:

酒精使用障碍对丙型肝炎患者失代偿期肝硬化的影响:一项国际研究
背景与目标 直接作用抗病毒药物 (DAA) 的出现已经为消除丙型肝炎病毒 (HCV) 制定了雄心勃勃的目标。然而,在酒精使用障碍的情况下,DAAs 实现这些目标的能力可能会受到影响。本研究的目的是评估酒精使用障碍在三种情况下对 HCV 相关失代偿性肝硬化的影响。方法 来自加拿大不列颠哥伦比亚省的 HCV 通报;新南威尔士州、澳大利亚和苏格兰(分别为 1995-2011/2012/2013)与住院(分别为 2001-2012/2013/2014)有关。酒精使用障碍被定义为因酒精使用而与肝脏无关的住院治疗。绘制了年龄标准化的失代偿期肝硬化发病率,使用 Cox 回归评估相关因素,和酒精使用障碍相关的人口归因分数(PAF)被计算出来。结果 在不列颠哥伦比亚、新南威尔士和苏格兰的 58,487、84,529 和 31,924 名 HCV 患者中,2,689 (4.6%)、3,169 (3.7%) 和 1,375 (4.3%) 有失代偿期肝硬化,诊断为 28% 32% 和 50% 的失代偿性肝硬化患者分别有酒精使用障碍。在新南威尔士州和苏格兰,酒精使用障碍患者的年龄标准化失代偿性肝硬化发病率要高得多。在不列颠哥伦比亚省 (aHR 1.92; 95% CI 1.76-2.10)、新南威尔士州 (aHR 3.68; 95% CI 3.38-4.00) 和苏格兰 (aHR 3.88; 95% CI 3.42-4.40),失代偿期肝硬化与酒精使用障碍独立相关)。与酒精使用障碍相关的失代偿期肝硬化的 PAF 分别为 13%、25%、不列颠哥伦比亚省、新南威尔士州和苏格兰分别为 40%。结论 酒精使用障碍是所有环境中 HCV 肝病负担的主要因素,在苏格兰更为明显。需要密切监测酒精使用会在多大程度上损害 DAA 治疗的个人和人群水平的益处。如果要实现世界卫生组织 2030 年降低 HCV 死亡率的目标,各国必须在适当的情况下制定战略,将促进 DAA 治疗与管理酒精使用障碍相结合。概述 全球丙型肝炎患者的肝脏疾病负担一直在增加。最近推出的针对丙型肝炎的高效药物(称为直接作用抗病毒药物或 DAA)为该行业带来了新的乐观情绪。DAA 的扩大可以消除丙型肝炎作为未来几十年的公共卫生威胁。然而,我们的研究结果表明,大量饮酒是丙型肝炎患者肝病的主要危险因素。如果继续,大量饮酒可能会损害新的抗病毒治疗在个人和人群层面的益处。为了在需要时将丙型肝炎作为公共卫生威胁来应对,DAA 治疗应与重度饮酒管理相结合。











































 京公网安备 11010802027423号
京公网安备 11010802027423号