JAMA Psychiatry ( IF 25.8 ) Pub Date : 2017-12-01 , DOI: 10.1001/jamapsychiatry.2017.3016 Yuri Milaneschi 1 , Femke Lamers 1 , Wouter J Peyrot 1 , Bernhard T Baune 2 , Gerome Breen 3, 4 , Abbas Dehghan 5 , Andreas J Forstner 6, 7, 8, 9, 10 , Hans J Grabe 11 , Georg Homuth 12 , Carol Kan 13, 14 , Cathryn Lewis 3 , Niamh Mullins 3 , Matthias Nauck 15, 16 , Giorgio Pistis 17 , Martin Preisig 17 , Margarita Rivera 3, 18 , Marcella Rietschel 19 , Fabian Streit 19 , Jana Strohmaier 19 , Alexander Teumer 20 , Sandra Van der Auwera 11 , Naomi R Wray 21, 22 , Dorret I Boomsma 23 , Brenda W J H Penninx 1 ,
|
Importance The association between major depressive disorder (MDD) and obesity may stem from shared immunometabolic mechanisms particularly evident in MDD with atypical features, characterized by increased appetite and/or weight (A/W) during an active episode.
Objective To determine whether subgroups of patients with MDD stratified according to the A/W criterion had a different degree of genetic overlap with obesity-related traits (body mass index [BMI] and levels of C-reactive protein [CRP] and leptin).
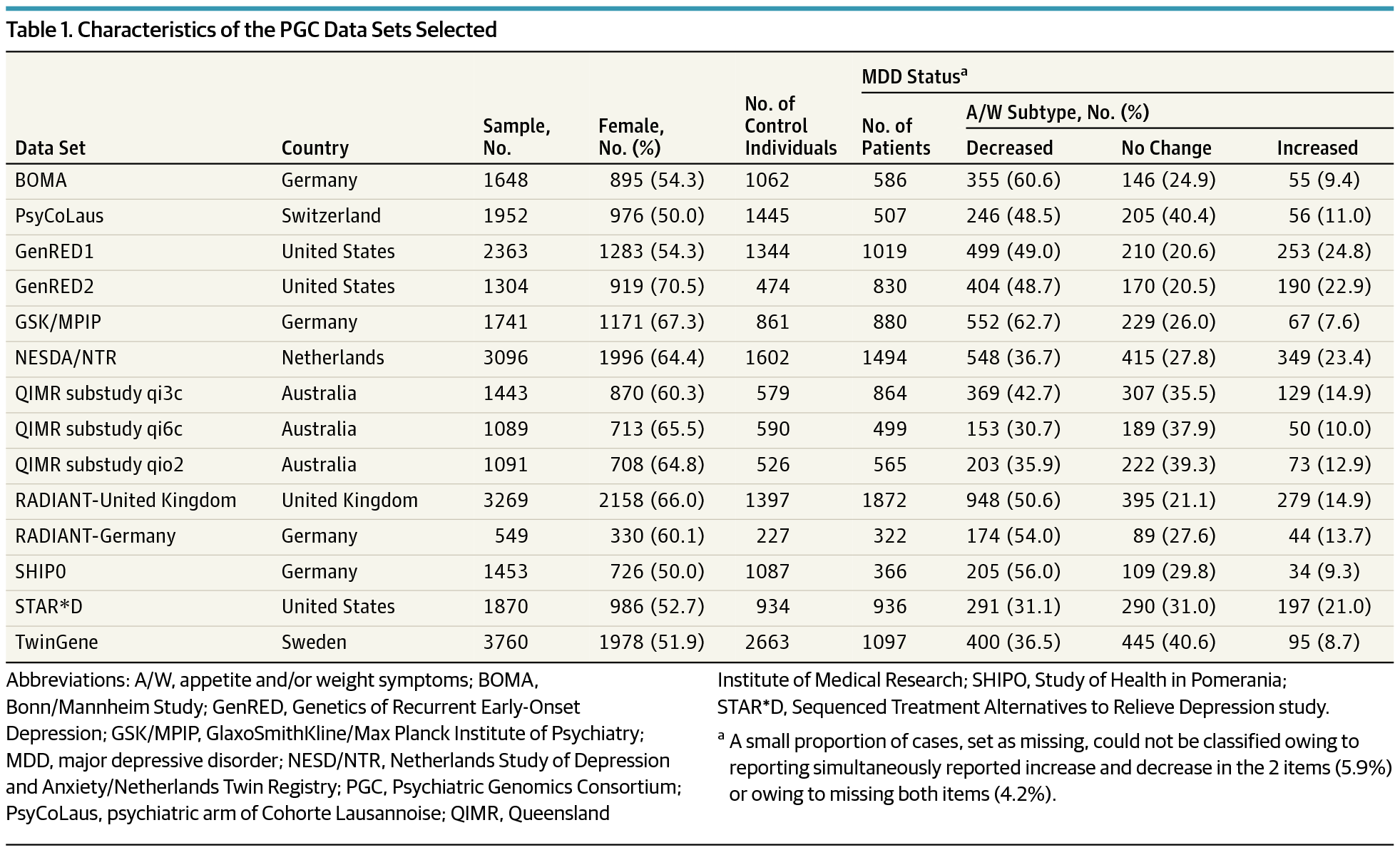
Design, Setting, and Patients This multicenter study assembled genome-wide genotypic and phenotypic measures from 14 data sets of the Psychiatric Genomics Consortium. Data sets were drawn from case-control, cohort, and population-based studies, including 26 628 participants with established psychiatric diagnoses and genome-wide genotype data. Data on BMI were available for 15 237 participants. Data were retrieved and analyzed from September 28, 2015, through May 20, 2017.
Main Outcomes and Measures Lifetime DSM-IV MDD was diagnosed using structured diagnostic instruments. Patients with MDD were stratified into subgroups according to change in the DSM-IV A/W symptoms as decreased or increased.
Results Data included 11 837 participants with MDD and 14 791 control individuals, for a total of 26 628 participants (59.1% female and 40.9% male). Among participants with MDD, 5347 (45.2%) were classified in the decreased A/W and 1871 (15.8%) in the increased A/W subgroups. Common genetic variants explained approximately 10% of the heritability in the 2 subgroups. The increased A/W subgroup showed a strong and positive genetic correlation (SE) with BMI (0.53 [0.15]; P = 6.3 × 10−4), whereas the decreased A/W subgroup showed an inverse correlation (−0.28 [0.14]; P = .06). Furthermore, the decreased A/W subgroup had a higher polygenic risk for increased BMI (odds ratio [OR], 1.18; 95% CI, 1.12-1.25; P = 1.6 × 10−10) and levels of CRP (OR, 1.08; 95% CI, 1.02-1.13; P = 7.3 × 10−3) and leptin (OR, 1.09; 95% CI, 1.06-1.12; P = 1.7 × 10−3).
Conclusions and Relevance The phenotypic associations between atypical depressive symptoms and obesity-related traits may arise from shared pathophysiologic mechanisms in patients with MDD. Development of treatments effectively targeting immunometabolic dysregulations may benefit patients with depression and obesity, both syndromes with important disability.
中文翻译:

重度抑郁症与非典型特征和肥胖相关免疫代谢失调的遗传关联
重要性 重度抑郁症 (MDD) 和肥胖之间的关联可能源于共同的免疫代谢机制,在具有非典型特征的 MDD 中尤为明显,其特征是在活动发作期间食欲和/或体重 (A/W) 增加。
目的 确定根据 A/W 标准分层的 MDD 患者亚组是否与肥胖相关特征(体重指数 [BMI] 和 C 反应蛋白 [CRP] 和瘦素水平)具有不同程度的遗传重叠。
设计、设置和患者 这项多中心研究从精神病学基因组学联盟的 14 个数据集中收集了全基因组的基因型和表型测量。数据集来自病例对照、队列和基于人群的研究,包括 26 628 名具有确定的精神病诊断和全基因组基因型数据的参与者。有 15 237 名参与者的 BMI 数据可用。从 2015 年 9 月 28 日到 2017 年 5 月 20 日,检索和分析了数据。
主要结果和措施 终生DSM-IV MDD 是使用结构化诊断仪器诊断的。根据DSM-IV A/W 症状的减少或增加,将 MDD 患者分层为亚组。
结果 数据包括 11 837 名 MDD 参与者和 14 791 名对照者,总共 26 628 名参与者(59.1% 女性和 40.9% 男性)。在患有 MDD 的参与者中,5347 名 (45.2%) 被归类为 A/W 下降亚组,1871 名 (15.8%) 被归类为 A/W 增加亚组。常见的遗传变异解释了 2 个亚组中大约 10% 的遗传力。增加的 A/W 亚组与 BMI(0.53 [0.15]; P = 6.3 × 10 -4 )显示出强烈的正遗传相关性(SE),而减少的 A/W 亚组显示出负相关(-0.28 [0.14] ; P = .06)。此外,降低的 A/W 亚组具有更高的 BMI 增加的多基因风险(优势比 [OR],1.18;95% CI,1.12-1.25;P = 1.6 × 10-10)和 CRP 水平(OR,1.08;95% CI,1.02-1.13;P = 7.3 × 10 -3)和瘦素(OR,1.09;95% CI,1.06-1.12;P = 1.7 × 10 -3)。
结论和相关性 非典型抑郁症状和肥胖相关性状之间的表型关联可能源于 MDD 患者的共同病理生理机制。开发有效针对免疫代谢失调的治疗方法可能会使抑郁症和肥胖症患者受益,这两种综合征都有严重的残疾。



























 京公网安备 11010802027423号
京公网安备 11010802027423号