Journal of Allergy and Clinical Immunology ( IF 11.4 ) Pub Date : 2017-09-27 , DOI: 10.1016/j.jaci.2017.07.052 Kyoung Yul Seo 1 , Kazuya Kitamura 2 , Soo Jung Han 3 , Brian Kelsall 4
|
Background
Dry eye disease (DED) affects one third of the population worldwide. In prior studies, experimental autoimmune lacrimal keratoconjunctivitis (EALK) induced by desiccating stress in mice has been used as a model of DED. This model is complicated by a requirement for exogenous epithelial cell injury and administration of anticholinergic agents with broad immunologic effects.
Objective
We sought to develop a novel mouse model of EALK and to demonstrate the responsible pathogenic mechanisms.
Methods
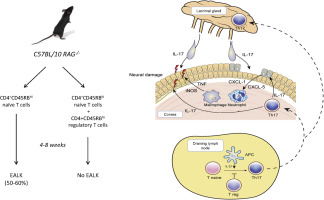
CD4+CD45RBhigh naive T cells with and without CD4+CD45RBlow regulatory T cells were adoptively transferred to C57BL/10 recombination-activating gene 2 (Rag2)−/− mice. The eyes, draining lymph nodes, lacrimal glands, and surrounding tissues of mice with and without spontaneous keratoconjunctivitis were evaluated for histopathologic changes, cellular infiltration, and cytokine production in tissues and isolated cells. Furthermore, the integrity of the corneal nerves was evaluated using whole-tissue immunofluorescence imaging. Gene-deficient naive T cells or RAG2-deficient hosts were evaluated to assess the roles of IFN-γ, IL-17A, and IL-23 in disease pathogenesis. Finally, cytokine levels were determined in the tears of patients with DED.
Results
EALK developed spontaneously in C57BL/10 Rag2−/− mice after adoptive transfer of CD4+CD45RBhigh naive T cells and was characterized by infiltration of CD4+ T cells, macrophages, and neutrophils. In addition to lacrimal keratoconjunctivitis, mice had damage to the corneal nerve, which connects components of the lacrimal functional unit. Pathogenic T-cell differentiation was dependent on IL-23p40 and controlled by cotransferred CD4+CD45RBlow regulatory T cells. TH17 rather than TH1 CD4+ cells were primarily responsible for EALK, even though levels of both IL-17 and IFN-γ were increased in inflammatory tissues, likely because of their ability to drive expression of CXC chemokines within the cornea and the subsequent influx of myeloid cells. Consistent with the findings of this model, the tears of patients with DED had increased levels of inflammatory cytokines, including IL-17A and TNF-α.
Conclusion
We describe a novel model of spontaneous EALK that supports a role for TH17 cells in disease pathogenesis and that will contribute to our understanding of autoimmune lacrimal keratoconjunctivitis in many human eye diseases, including DED.
中文翻译:

TH17 细胞在伴有神经损伤的自发实验性自身免疫性泪角结膜炎新模型中介导炎症
背景
干眼症(DED)影响着全世界三分之一的人口。在之前的研究中,小鼠干燥应激诱导的实验性自身免疫性泪道角结膜炎(EALK)已被用作 DED 模型。该模型由于需要外源性上皮细胞损伤和施用具有广泛免疫作用的抗胆碱能药物而变得复杂。
客观的
我们试图开发一种新型 EALK 小鼠模型并证明其致病机制。
方法
将具有和不具有CD4 + CD45RB低调节T细胞的CD4 + CD45RB高初始T细胞过继转移至C57BL/10重组激活基因2 (Rag2) -/−小鼠。对患有和不患有自发性角结膜炎的小鼠的眼睛、引流淋巴结、泪腺和周围组织的组织病理学变化、细胞浸润以及组织和分离细胞中细胞因子的产生进行评估。此外,使用全组织免疫荧光成像评估角膜神经的完整性。对基因缺陷的初始 T 细胞或 RAG2 缺陷的宿主进行评估,以评估 IFN-γ、IL-17A 和 IL-23 在疾病发病机制中的作用。最后,测定了 DED 患者眼泪中的细胞因子水平。
结果
EALK 在 CD4 + CD45RB高幼稚 T 细胞过继转移后在 C57BL/10 Rag2 −/−小鼠中自发发育,其特征是 CD4 + T 细胞、巨噬细胞和中性粒细胞浸润。除了泪道角结膜炎之外,小鼠的角膜神经也受到损伤,角膜神经连接泪道功能单元的各个组成部分。致病性 T 细胞分化依赖于 IL-23p40,并由共转移的 CD4 + CD45RB低调节 T 细胞控制。 T H 17 而不是 T H 1 CD4 +细胞是 EALK 的主要原因,尽管炎症组织中 IL-17 和 IFN-γ 的水平均增加,这可能是因为它们能够驱动角膜内 CXC 趋化因子的表达,并且随后骨髓细胞的涌入。与该模型的研究结果一致,DED 患者的眼泪中炎症细胞因子的水平升高,包括 IL-17A 和 TNF-α。
结论
我们描述了一种自发性 EALK 的新模型,该模型支持 T H 17 细胞在疾病发病机制中的作用,并将有助于我们了解许多人类眼部疾病(包括 DED)中的自身免疫性泪道角结膜炎。











































 京公网安备 11010802027423号
京公网安备 11010802027423号