JAMA Oncology ( IF 22.5 ) Pub Date : 2018-01-01 , DOI: 10.1001/jamaoncol.2017.2993 Matthew P Smeltzer 1 , Nicholas R Faris 2 , Meredith A Ray 1 , Raymond U Osarogiagbon 2
|
Importance Pathologic nodal stage is the most significant prognostic factor in resectable non–small cell lung cancer (NSCLC). The International Association for the Study of Lung Cancer NSCLC staging project revealed intercontinental differences in N category–stratified survival. These differences may indicate differences not only in cancer biology but also in the thoroughness of the nodal examination.
Objective To determine whether survival was affected by sequentially more stringent definitions of pN staging quality in a cohort of patients with NSCLC after resection with curative intent.
Design This observational study used the Mid-South Quality of Surgical Resection cohort, a population-based database of lung cancer resections with curative intent. A total of 2047 consecutive patients who underwent surgical resection at 11 hospitals with at least 5 annual lung cancer resections in 4 contiguous US Dartmouth hospital referral regions in northern Mississippi, eastern Arkansas, and western Tennessee (>90% of the eligible population) were included. Resections were performed from January 1, 2009, through January 25, 2016. Survival was evaluated with the Kaplan-Meier method and Cox proportional hazards models.
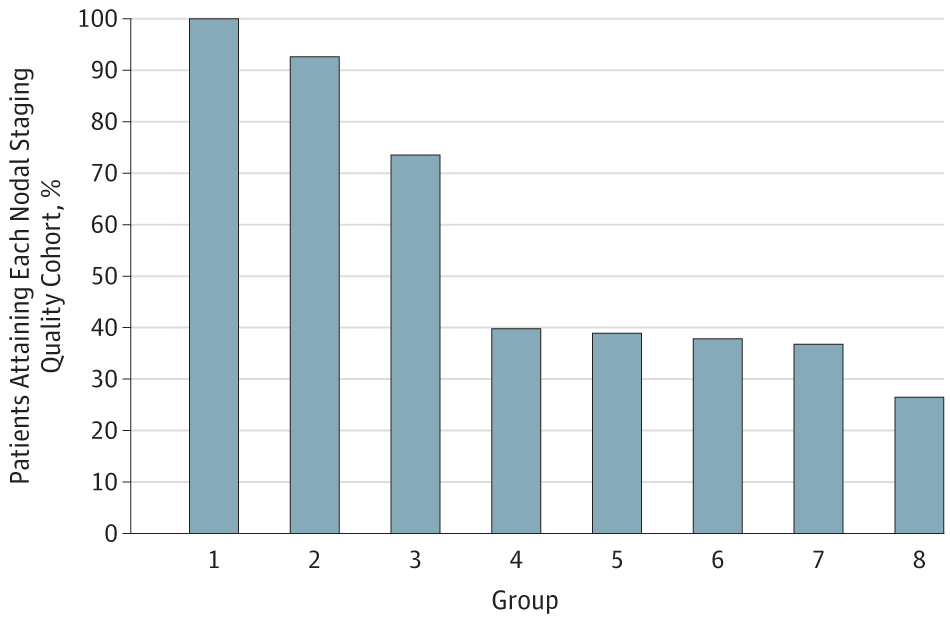
Exposures Eight sequentially more stringent pN staging quality strata included the following: all patients (group 1); those with complete resections only (group 2); those with examination of at least 1 mediastinal lymph node (group 3); those with examination of at least 10 lymph nodes (group 4); those with examination of at least 3 hilar or intrapulmonary and at least 3 mediastinal lymph nodes (group 5); those with examination of at least 10 lymph nodes, including at least 1 mediastinal lymph node (group 6); those with examination of at least 1 hilar or intrapulmonary and at least 3 mediastinal nodal stations (group 7); and those with examination of at least 1 hilar or intrapulmonary lymph node, at least 10 total lymph nodes, and at least 3 mediastinal nodal stations (group 8).
Main Outcomes and Measures N category–stratified overall survival.
Results Of the total 2047 patients (1046 men [51.1%] and 1001 women [48.9%]; mean [SD] age, 67.0 [9.6] years) included in the analysis, the eligible analysis population ranged from 541 to 2047, depending on stringency. Sequential improvement in the N category–stratified 5-year survival of pN0 and pN1 tumors was found from the least stringent group (0.63 [95% CI, 0.59-0.66] for pN0 vs 0.46 [95% CI, 0.38-0.54] for pN1) to the most stringent group (0.71 [95% CI, 0.60-0.79] for pN0 vs 0.60 [95% CI, 0.43-0.73] for pN1). The pN1 cohorts with 3 or more mediastinal nodal stations examined had the most striking survival improvements. More stringently defined mediastinal nodal examination was associated with better separation in survival curves between patients with pN1 and pN2 tumors.
Conclusions and Relevance The prognostic value of pN stratification depends on the thoroughness of examination. Differences in thoroughness of nodal staging may explain a large proportion of intercontinental survival differences. More thorough nodal examination practice must be disseminated to improve the prognostic value of the TNM staging system. Future updates of the TNM staging system should incorporate more quality restraints.
中文翻译:

非小细胞肺癌根治性切除术后病理淋巴结分期质量与生存率的关系
重要性 病理淋巴结分期是可切除非小细胞肺癌 (NSCLC) 最重要的预后因素。国际肺癌研究协会 NSCLC 分期项目揭示了 N 类分层生存期的洲际差异。这些差异可能表明不仅在癌症生物学方面存在差异,而且在淋巴结检查的彻底性方面也存在差异。
目的 确定在以治愈为目的的非小细胞肺癌患者队列中,对 pN 分期质量的顺序更严格的定义是否会影响生存率。
设计 这项观察性研究使用了中南部手术切除质量队列,这是一个基于人群的具有治愈目的的肺癌切除数据库。在密西西比州北部、阿肯色州东部和田纳西州西部的 4 个连续的美国达特茅斯医院转诊区(>90% 的合格人群),共有 2047 名连续患者在 11 家医院接受了手术切除,每年至少进行 5 次肺癌切除术. 切除手术于 2009 年 1 月 1 日至 2016 年 1 月 25 日进行。使用 Kaplan-Meier 方法和 Cox 比例风险模型评估存活率。
暴露 八个依次更严格的 pN 分期质量层包括以下内容:所有患者(第 1 组);仅完全切除的患者(第 2 组);检查至少 1 个纵隔淋巴结的患者(第 3 组);检查至少 10 个淋巴结的患者(第 4 组);检查至少 3 个肺门或肺内和至少 3 个纵隔淋巴结的患者(第 5 组);检查至少 10 个淋巴结的患者,包括至少 1 个纵隔淋巴结(第 6 组);检查至少 1 个肺门或肺内和至少 3 个纵隔淋巴结站的患者(第 7 组);检查至少 1 个肺门或肺内淋巴结、至少 10 个总淋巴结和至少 3 个纵隔淋巴结站(第 8 组)。
主要结果和测量 N 类分层的总生存期。
结果 在分析中纳入的 2047 名患者(1046 名男性 [51.1%] 和 1001 名女性 [48.9%];平均 [SD] 年龄,67.0 [9.6] 岁)中,符合条件的分析人群范围为 541 至 2047,具体取决于严格性。从最不严格的组中发现,pN0 和 pN1 肿瘤的 N 类分层 5 年生存率连续改善(pN0 为 0.63 [95% CI,0.59-0.66] vs pN1 为 0.46 [95% CI,0.38-0.54] ) 到最严格的组(pN0 为 0.71 [95% CI, 0.60-0.79] 与 pN1 为 0.60 [95% CI, 0.43-0.73])。具有 3 个或更多纵隔淋巴结站点的 pN1 队列具有最显着的生存改善。更严格定义的纵隔淋巴结检查与 pN1 和 pN2 肿瘤患者之间生存曲线的更好分离相关。
结论和相关性 pN 分层的预后价值取决于检查的彻底性。淋巴结分期彻底性的差异可以解释大部分洲际生存差异。必须传播更彻底的淋巴结检查实践,以提高 TNM 分期系统的预后价值。TNM 分期系统的未来更新应该包含更多的质量限制。









































 京公网安备 11010802027423号
京公网安备 11010802027423号