当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Premature ovarian senescence and high miscarriage rate impair fertility in women with hepatitis C virus infection
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-01-01 , DOI: 10.1016/j.jhep.2017.08.019 Aimilia Karampatou 1 , Xue Han 2 , Loreta A Kondili 3 , Gloria Taliani 4 , Alessia Ciancio 5 , Filomena Morisco 6 , Rosina Maria Critelli 1 , Enrica Baraldi 7 , Veronica Bernabucci 1 , Giulia Troshina 5 , Maria Guarino 6 , Simonetta Tagliavini 7 , Federica D'Ambrosio 1 , Laura Bristot 1 , Laura Turco 1 , Stefano Rosato 3 , Stefano Vella 3 , Tommaso Trenti 7 , Isabella Neri 8 , Antonio La Marca 8 , Shivaji Manthena 9 , Andrea S Goldstein 9 , Savino Bruno 10 , Yanjun Bao 9 , Yuri Sanchez Gonzalez 9 , Erica Villa 1 , ,
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-01-01 , DOI: 10.1016/j.jhep.2017.08.019 Aimilia Karampatou 1 , Xue Han 2 , Loreta A Kondili 3 , Gloria Taliani 4 , Alessia Ciancio 5 , Filomena Morisco 6 , Rosina Maria Critelli 1 , Enrica Baraldi 7 , Veronica Bernabucci 1 , Giulia Troshina 5 , Maria Guarino 6 , Simonetta Tagliavini 7 , Federica D'Ambrosio 1 , Laura Bristot 1 , Laura Turco 1 , Stefano Rosato 3 , Stefano Vella 3 , Tommaso Trenti 7 , Isabella Neri 8 , Antonio La Marca 8 , Shivaji Manthena 9 , Andrea S Goldstein 9 , Savino Bruno 10 , Yanjun Bao 9 , Yuri Sanchez Gonzalez 9 , Erica Villa 1 , ,
Affiliation
|
BACKGROUND & AIMS
Premenopausal women who are HCV positive (HCV+) have failing ovarian function, which is likely to impact their fertility. Thus, we investigated the reproductive history, risk of infertility, and pregnancy outcomes in women of childbearing age who were HCV+. METHODS
Three different groups were studied: (1) Clinical cohort: 100 women who were HCV+ and also had chronic liver disease (CLD), age matched with 50 women who were HBV+ with CLD and with 100 healthy women; all women were consecutively observed in three gastroenterology units in hospitals in Italy; (2) 1,998 women who were HCV+ and enrolled in the Italian Platform for the Study of Viral Hepatitis Therapies (PITER); (3) 6,085 women, who were mono-infected with HCV, and 20,415 women, who were HCV-, from a large de-identified insurance database from the USA. MEASUREMENTS
total fertility rate (TFR) defined as the average number of children that a woman would bear during her lifetime. To define the reproductive stage of each participant, levels of anti-Müllerian hormone (AMH) and 17β-estradiol were measured. RESULTS
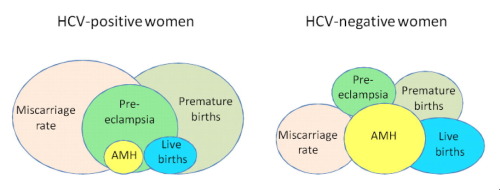
Clinical cohort: women who were either HCV+ or HBV+ had similar CLD severity and age at first pregnancy. Based on a multivariate analysis, women who were HCV+ had a higher risk of miscarriage than those who were HBV+ (odds ratio [OR] 6,905; 95% CI 1.771-26.926). Among women who were HCV+, incidence of miscarriage was correlated with median AMH level (1.0 ng/ml). Achieving a sustained virologic response (SVR) after antiviral treatment reduced the risk of miscarriage (OR 0.255; 95% CI 0.090-0.723). In the PITER-HCV cohort, miscarriage occurred in 42.0% of women (44.6% had multiple miscarriages). TFR for women who were HCV+ and between 15 and 49 years of age was 0.7 vs. 1.37 of Italian population of the same age range. In the US cohort: compared with women who were HCV-, women who were HCV+ positive were significantly more likely to have infertility (OR 2.439; 95% CI 2.130-2.794), premature birth (OR 1.34; 95% CI 1.060-1.690), gestational diabetes (OR 1.24; 95% CI 1.020-1.510), and pre-eclampsia (OR 1.206; 95% CI 0.935-1.556), and were less likely to have a live birth (OR 0.754; 95% CI 0.622-0.913). CONCLUSIONS
Ovarian senescence in women of childbearing age who are HCV+ is associated with a lower chance of live birth, greater risk of infertility, gestational diabetes, pre-eclampsia and miscarriage. Such risks could be positively influenced by successful HCV cure. LAY SUMMARY
Most new cases of HCV infection are among people who inject drugs, many of whom are young women in their childbearing years. Women of reproductive age who are HCV+ display markers of ovarian senescence. This is associated with an increased burden in terms of infertility and adverse pregnancy outcomes, including stillbirth, miscarriage, fewer live births, and gestational diabetes. Early viral suppression with therapy is likely to mitigate these risks.
中文翻译:

卵巢过早衰老和高流产率损害丙型肝炎病毒感染女性的生育能力
背景与目标 HCV 阳性 (HCV+) 的绝经前女性卵巢功能衰竭,这可能会影响她们的生育能力。因此,我们调查了 HCV + 育龄妇女的生育史、不孕风险和妊娠结局。方法 研究了三个不同的组: (1) 临床队列:100 名 HCV + 并患有慢性肝病 (CLD) 的女性,年龄与 50 名 HBV + 患有 CLD 的女性和 100 名健康女性相匹配;所有女性均在意大利医院的三个胃肠病科连续接受观察; (2) 1,998 名 HCV+ 女性并参加了意大利病毒性肝炎治疗研究平台 (PITER); (3) 来自美国大型去识别化保险数据库的 6,085 名 HCV 单一感染女性和 20,415 名 HCV 阴性女性。衡量指标 总生育率 (TFR) 定义为女性一生中平均生育的孩子数量。为了确定每个参与者的生殖阶段,测量了抗苗勒管激素 (AMH) 和 17β-雌二醇的水平。结果 临床队列:HCV+ 或 HBV+ 女性的 CLD 严重程度和首次怀孕时的年龄相似。根据多变量分析,HCV + 女性的流产风险高于 HBV + 女性(比值比 [OR] 6,905;95% CI 1.771-26.926)。在 HCV+ 的女性中,流产发生率与中位 AMH 水平(1.0 ng/ml)相关。抗病毒治疗后实现持续病毒学应答(SVR)可降低流产风险(OR 0.255;95% CI 0.090-0.723)。在 PITER-HCV 队列中,42.0% 的女性发生流产(44.6% 多次流产)。 15 岁至 49 岁之间 HCV+ 女性的 TFR 分别为 0.7 和 1。37 意大利同年龄段人口。在美国队列中:与 HCV- 女性相比,HCV+ 阳性女性更容易出现不孕症(OR 2.439;95% CI 2.130-2.794)、早产(OR 1.34;95% CI 1.060-1.690) 、妊娠糖尿病(OR 1.24;95% CI 1.020-1.510)和先兆子痫(OR 1.206;95% CI 0.935-1.556),并且活产的可能性较小(OR 0.754;95% CI 0.622-0.913) )。结论 HCV + 育龄妇女的卵巢衰老与活产机会降低、不孕、妊娠期糖尿病、先兆子痫和流产风险增加相关。成功治愈丙肝病毒可能会对此类风险产生积极影响。简要摘要 大多数丙肝病毒感染新病例发生在注射吸毒者中,其中许多是育龄期的年轻女性。 HCV+ 的育龄女性表现出卵巢衰老的标志。这与不孕和不良妊娠结局的负担增加有关,包括死产、流产、活产减少和妊娠糖尿病。早期通过治疗抑制病毒可能会减轻这些风险。
更新日期:2018-01-01
中文翻译:

卵巢过早衰老和高流产率损害丙型肝炎病毒感染女性的生育能力
背景与目标 HCV 阳性 (HCV+) 的绝经前女性卵巢功能衰竭,这可能会影响她们的生育能力。因此,我们调查了 HCV + 育龄妇女的生育史、不孕风险和妊娠结局。方法 研究了三个不同的组: (1) 临床队列:100 名 HCV + 并患有慢性肝病 (CLD) 的女性,年龄与 50 名 HBV + 患有 CLD 的女性和 100 名健康女性相匹配;所有女性均在意大利医院的三个胃肠病科连续接受观察; (2) 1,998 名 HCV+ 女性并参加了意大利病毒性肝炎治疗研究平台 (PITER); (3) 来自美国大型去识别化保险数据库的 6,085 名 HCV 单一感染女性和 20,415 名 HCV 阴性女性。衡量指标 总生育率 (TFR) 定义为女性一生中平均生育的孩子数量。为了确定每个参与者的生殖阶段,测量了抗苗勒管激素 (AMH) 和 17β-雌二醇的水平。结果 临床队列:HCV+ 或 HBV+ 女性的 CLD 严重程度和首次怀孕时的年龄相似。根据多变量分析,HCV + 女性的流产风险高于 HBV + 女性(比值比 [OR] 6,905;95% CI 1.771-26.926)。在 HCV+ 的女性中,流产发生率与中位 AMH 水平(1.0 ng/ml)相关。抗病毒治疗后实现持续病毒学应答(SVR)可降低流产风险(OR 0.255;95% CI 0.090-0.723)。在 PITER-HCV 队列中,42.0% 的女性发生流产(44.6% 多次流产)。 15 岁至 49 岁之间 HCV+ 女性的 TFR 分别为 0.7 和 1。37 意大利同年龄段人口。在美国队列中:与 HCV- 女性相比,HCV+ 阳性女性更容易出现不孕症(OR 2.439;95% CI 2.130-2.794)、早产(OR 1.34;95% CI 1.060-1.690) 、妊娠糖尿病(OR 1.24;95% CI 1.020-1.510)和先兆子痫(OR 1.206;95% CI 0.935-1.556),并且活产的可能性较小(OR 0.754;95% CI 0.622-0.913) )。结论 HCV + 育龄妇女的卵巢衰老与活产机会降低、不孕、妊娠期糖尿病、先兆子痫和流产风险增加相关。成功治愈丙肝病毒可能会对此类风险产生积极影响。简要摘要 大多数丙肝病毒感染新病例发生在注射吸毒者中,其中许多是育龄期的年轻女性。 HCV+ 的育龄女性表现出卵巢衰老的标志。这与不孕和不良妊娠结局的负担增加有关,包括死产、流产、活产减少和妊娠糖尿病。早期通过治疗抑制病毒可能会减轻这些风险。











































 京公网安备 11010802027423号
京公网安备 11010802027423号