当前位置:
X-MOL 学术
›
ACS Biomater. Sci. Eng.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
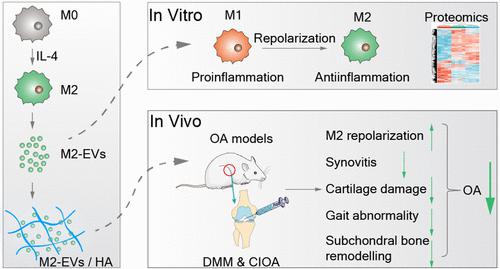
M2 Macrophage-Derived Extracellular Vesicles Encapsulated in Hyaluronic Acid Alleviate Osteoarthritis by Modulating Macrophage Polarization
ACS Biomaterials Science & Engineering ( IF 5.8 ) Pub Date : 2024-04-02 , DOI: 10.1021/acsbiomaterials.3c01833 Qiling Yuan 1 , Mingyi Yang 1 , Haishi Zheng 1 , Yongsong Cai 1 , Pan Luo 1 , Xinyi Wang 2 , Peng Xu 1
ACS Biomaterials Science & Engineering ( IF 5.8 ) Pub Date : 2024-04-02 , DOI: 10.1021/acsbiomaterials.3c01833 Qiling Yuan 1 , Mingyi Yang 1 , Haishi Zheng 1 , Yongsong Cai 1 , Pan Luo 1 , Xinyi Wang 2 , Peng Xu 1
Affiliation
|
An imbalance between M1 and M2 macrophage polarization is critical in osteoarthritis (OA) development. We investigated the effect of M2 macrophage-derived extracellular vesicles (M2-EVs) to reprogramme macrophages from the M1 to M2 phenotype for OA treatment. M1 macrophages and mouse OA models were treated with M2-EVs. Proteomic analysis was performed to evaluate macrophage polarization in vitro. The OA models were as follows: destabilization of the medial meniscus (DMM) surgery-induced OA and collagenase-induced OA (CIOA). Hyaluronic acid (HA) was used to deliver M2-EVs. M2-EVs decreased macrophage accumulation, repolarized macrophages from the M1 to M2 phenotype, mitigated synovitis, reduced cartilage degradation, alleviated subchondral bone damage, and improved gait abnormalities in the CIOA and DMM models. Moreover, HA increased the retention time of M2-EVs and enhanced the efficiency of M2-EVs in OA treatment. Furthermore, proteomic analysis demonstrated that M2-EVs exhibited a macrophage reprogramming ability similar to IL-4, and the pathways might be the NOD-like receptor (NLR), TNF, NF-κB, and Toll-like receptor (TLR) signaling pathways. M2-EVs reprogrammed macrophages from the M1 to M2 phenotype, which resulted in beneficial effects on cartilage and attenuation of OA severity. In summary, our study indicated that M2-EV-guided reprogramming of macrophages is a promising treatment strategy for OA.
中文翻译:

封装在透明质酸中的 M2 巨噬细胞衍生的细胞外囊泡通过调节巨噬细胞极化减轻骨关节炎
M1 和 M2 巨噬细胞极化之间的不平衡对于骨关节炎 (OA) 的发展至关重要。我们研究了 M2 巨噬细胞衍生的细胞外囊泡 (M2-EV) 将巨噬细胞从 M1 表型重编程为 M2 表型以治疗 OA 的作用。 M1 巨噬细胞和小鼠 OA 模型用 M2-EV 处理。进行蛋白质组分析以评估体外巨噬细胞极化。 OA模型如下:内侧半月板不稳定(DMM)手术诱发的OA和胶原酶诱发的OA(CIOA)。透明质酸 (HA) 用于输送 M2-EV。在 CIOA 和 DMM 模型中,M2-EV 减少了巨噬细胞的积累,使巨噬细胞从 M1 表型重新极化为 M2 表型,减轻了滑膜炎,减少了软骨退化,减轻了软骨下骨损伤,并改善了步态异常。此外,HA增加了M2-EV的保留时间并提高了M2-EV在OA治疗中的效率。此外,蛋白质组学分析表明,M2-EVs表现出类似于IL-4的巨噬细胞重编程能力,其通路可能是NOD样受体(NLR)、TNF、NF-κB和Toll样受体(TLR)信号通路。 M2-EV 将巨噬细胞从 M1 表型重新编程为 M2 表型,这对软骨产生有益影响并减轻 OA 严重程度。总之,我们的研究表明,M2-EV 引导的巨噬细胞重编程是一种有前景的 OA 治疗策略。
更新日期:2024-04-02
中文翻译:

封装在透明质酸中的 M2 巨噬细胞衍生的细胞外囊泡通过调节巨噬细胞极化减轻骨关节炎
M1 和 M2 巨噬细胞极化之间的不平衡对于骨关节炎 (OA) 的发展至关重要。我们研究了 M2 巨噬细胞衍生的细胞外囊泡 (M2-EV) 将巨噬细胞从 M1 表型重编程为 M2 表型以治疗 OA 的作用。 M1 巨噬细胞和小鼠 OA 模型用 M2-EV 处理。进行蛋白质组分析以评估体外巨噬细胞极化。 OA模型如下:内侧半月板不稳定(DMM)手术诱发的OA和胶原酶诱发的OA(CIOA)。透明质酸 (HA) 用于输送 M2-EV。在 CIOA 和 DMM 模型中,M2-EV 减少了巨噬细胞的积累,使巨噬细胞从 M1 表型重新极化为 M2 表型,减轻了滑膜炎,减少了软骨退化,减轻了软骨下骨损伤,并改善了步态异常。此外,HA增加了M2-EV的保留时间并提高了M2-EV在OA治疗中的效率。此外,蛋白质组学分析表明,M2-EVs表现出类似于IL-4的巨噬细胞重编程能力,其通路可能是NOD样受体(NLR)、TNF、NF-κB和Toll样受体(TLR)信号通路。 M2-EV 将巨噬细胞从 M1 表型重新编程为 M2 表型,这对软骨产生有益影响并减轻 OA 严重程度。总之,我们的研究表明,M2-EV 引导的巨噬细胞重编程是一种有前景的 OA 治疗策略。



























 京公网安备 11010802027423号
京公网安备 11010802027423号